Airway Management with Point-of-Care-Ultrasound: A Breath of Fresh Air
EMS just alerted you that a cardiac arrest is en route. You now have three minutes to gather all your airway equipment. You call respiratory therapy, get your oxygen and suction set up, and grab your tube, blade, lube, and syringe. Just in case, you grab your GlideScope and bougie. Did you grab your ultrasound? Sure, you probably grabbed it to assess cardiac activity, but what about the airway? The patient is brought in with an endotracheal tube already in place. You go to listen for breath sounds but with all of the chaos around, the airway is difficult to assess with your stethoscope alone. Quite frankly, you cannot hear anything, and the EtCO2 will take a couple of minutes to get set up.
Now consider another scenario. A young woman just had a first date at a Red Lobster and in trying to impress her date, ate some lobster even though she knows she is allergic. She comes into your critical care area with a large amount of angioedema, with stridor, hypotensive, and covered in hives. You order the anaphylaxis medications and while the nurse is grabbing the medications, you quickly grab an eleven blade, a boogie, and a 6.0 endotracheal tube because you have a sick feeling in your stomach telling you where this is headed. You start palpating the neck for landmarks and quite frankly, this is a disaster—she is female, has a short neck, is obese, and with all the swelling, you really have no idea what you are feeling.
In both situations, what do you do? After reading this article, I hope you will grab your linear probe.
Endotracheal Intubation
POCUS can be utilized to determine correct tube position either by direct visualization of the tube in the trachea or esophagus or indirectly by assessing ventilation, either by detecting pleural sliding or diaphragmatic excursion.
Esophageal intubations might occur as often as 15.3% of the time during emergency airway access. [1] Traditionally, auscultation is the preferred method of excluding esophageal intubation but it takes time, increases the risk of aspiration, and is relatively unreliable. [2] EtCO2 is the gold standard for confirming tube placement; however, this too can be unreliable, particularly in cardiac arrest when it is only 60% to 65% sensitive for identifying endotracheal intubations. [3]
One of the first studies to look at point-of-care ultrasound (POCUS) confirmation of tracheal intubation found that it was accurate 98.2% of the time with a kappa value of 0.93, which aligns highly with capnography confirmation. [4] A large meta-analysis of seventeen studies and 1,595 patients showed that POCUS was 98.7% sensitive and 97.1% specific. [1] A more recent meta-analysis with 30 studies and 2,534 patients showed that POCUS was 98.2% sensitive and 95.7% specific. [5] A study conducted in the emergency department at a Level I trauma center showed that the dynamic POCUS approach took an average of 18.25 seconds to identify esophageal intubations compared to the 177.5 seconds that it took in the EtCO2 group. [2]
Tube Confirmation Method
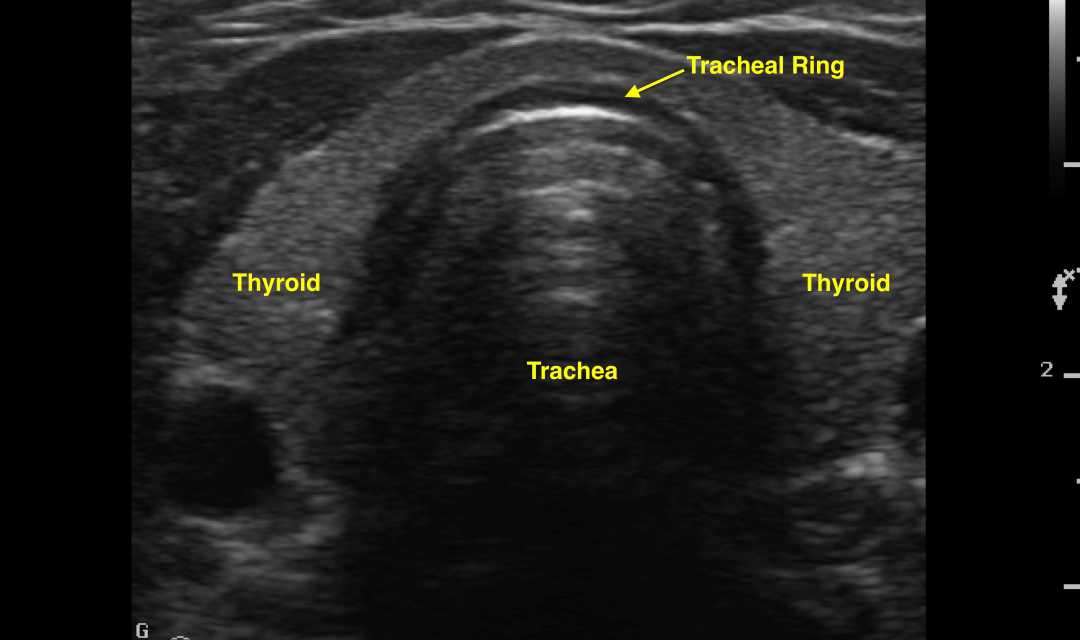
Step 1: Place the linear probe in a transverse plane superior to the suprasternal notch to visualize the trachea (Fig. 1). The esophagus may appear as a thick five-layered structure usually on the left of the trachea. Note the thyroid lobes and isthmus.
Step 2: In a tracheal intubation you will see one air-mucosal interface with a comet-tail artifact and posterior shadowing. However, if the intubation is esophageal, you will see two air-mucosal interfaces (“double tract sign”) with the comet-tail artifact and posterior shadowing. This double tract sign has a sensitivity of 98% and specificity of 95% for esophageal intubation. [2]
Step 3: Next, use the same probe to check the lungs bilaterally for lung sliding. Absence of lung sliding on the left indicates a right main stem intubation, and the tube will need to be pulled back (Fig. 2).
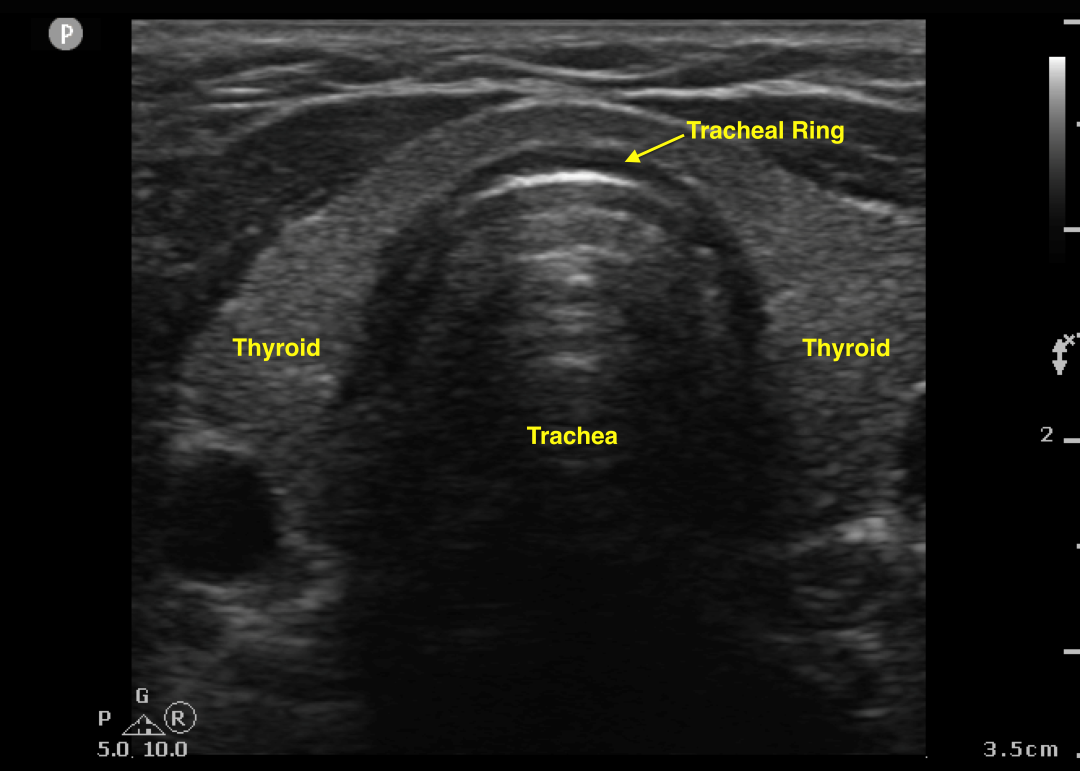
Fig 1: Trachea, transverse plane, at level of sternal notch.
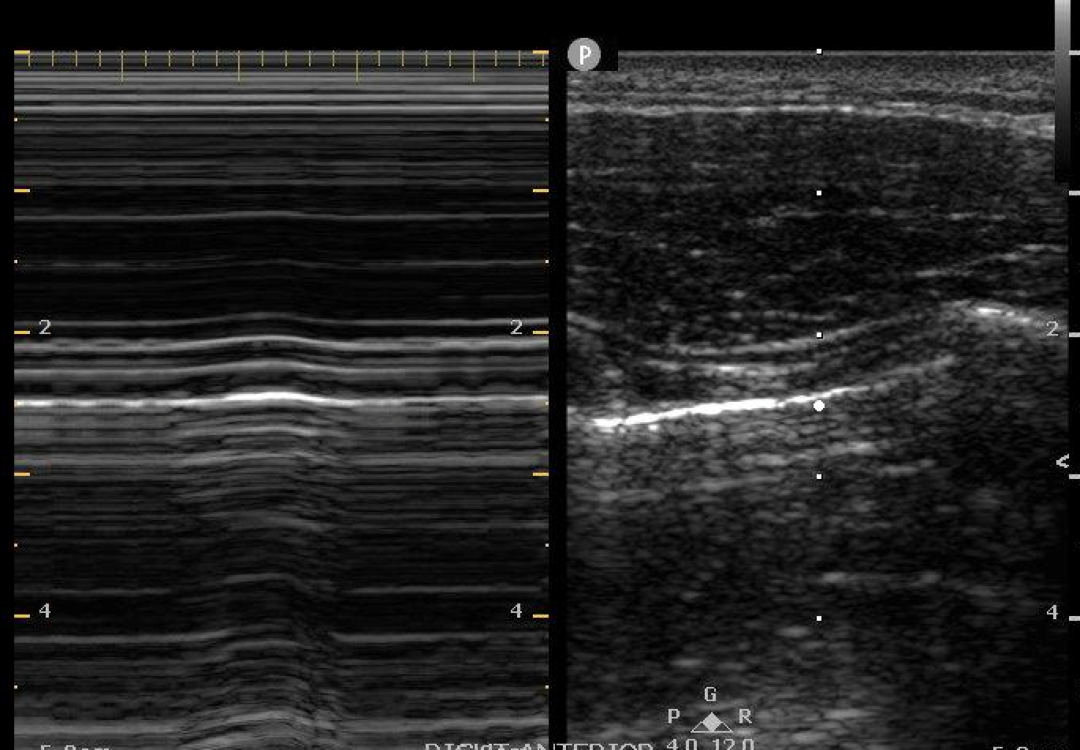
Fig 2: Bar-code sign on M-mode confirming absence of lung sliding.
HOT TIP: You can confirm the depth of the tube by placing saline or air into the tube balloon cuff. Now when scanning in the longitudinal plane, the tube may easily be visualized. Location of the balloon at the sternal notch correlates to the correct tube depth.
Cricothyrotomy
The standard method for identification of the cricothyroid membrane (CTM) is the landmark palpation technique. This involves palpating the midline skin between the cricoid cartilage and the thyroid cartilage; however, this is only accurate 62% of the time. [6] Identifying the CTM is often even more difficult in patients with obesity, short neck, subcutaneous emphysema, prior neck surgeries or radiation, or in female patients. [6]
Research has shown POCUS to be very useful. In cadavers with difficult or impossible landmark palpitation, POCUS resulted in a 5.6 times improvement in securing the surgical airway.6 On one female patient with a BMI of 45.3 with a two-minute limit, anesthesiologists using the landmark technique were successful 37% of the time compared to 83% of the time with ultrasound. [6]
Thus, experts have strongly recommended using POCUS to identify and mark the CTM prior to performing a needle or standard cricothyrotomy.
There are two techniques to locate the CTM: the string of pearls method in the longitudinal plane and the Thyroid-Air-Cricoid-Air (TACA) method in the transverse plane. In both techniques, the patient should be placed in the supine position with the neck extended.
Longitudinal String of Pearls Method
Step 1: Place the linear probe in the transverse plane at the level of the sternal notch (Fig. 1).
Step 2: Next, move the probe towards the left and bisect the trachea with the right edge of the image (Fig. 3).
Step 3: Rotate the probe into the longitudinal plane and visualize the ‘string of pearls’ appearance of tracheal rings, which will appear as dark, anechoic structures anterior to a white, hyperechoic line (Fig. 4).
Step 4: Slide the probe towards the patient’s head to find the cricoid cartilage and the thyroid cartilage. The CTM lies between the thyroid cartilage and the cricoid cartilage (Fig. 5). Mark this point on the skin. Perform a standard cricothyrotomy procedure.
Transverse TACA Method
Step 1: Place the linear probe in the transverse plane at the level of the sternal notch to visualize the trachea (Fig. 1). Slide cranially to locate the V shaped thyroid cartilage (T), which is visualized as a triangular pointy structure, like Mount Fuji (Fig. 6).
Step 2: Continue sliding caudally toward the patient’s toes to reveal air (A) as a hyperechoic white line with posterior reverberation artifacts (A-lines). This crater is the CTM (Fig. 7).
Step 3: Slide towards the patient’s toes until the cricoid cartilage (C) appears as a hypoechoic round arch-shaped structure, like Ayers rock (Fig. 8).
Step 4: Slide back cranially to confirm air (A), which is the CTM is located between the thyroid and cricoid cartilage. Mark the CTM on the skin. Perform a standard cricothyrotomy procedure (Fig. 7).
Summary
It is my hope that I have convinced you to grab your linear probe before you grab your stethoscope or phone to call for an expedited portable chest x-ray. With practice, POCUS can be a powerful tool in your airway crash cart. Relax, and take a deep breath with POCUS. ■
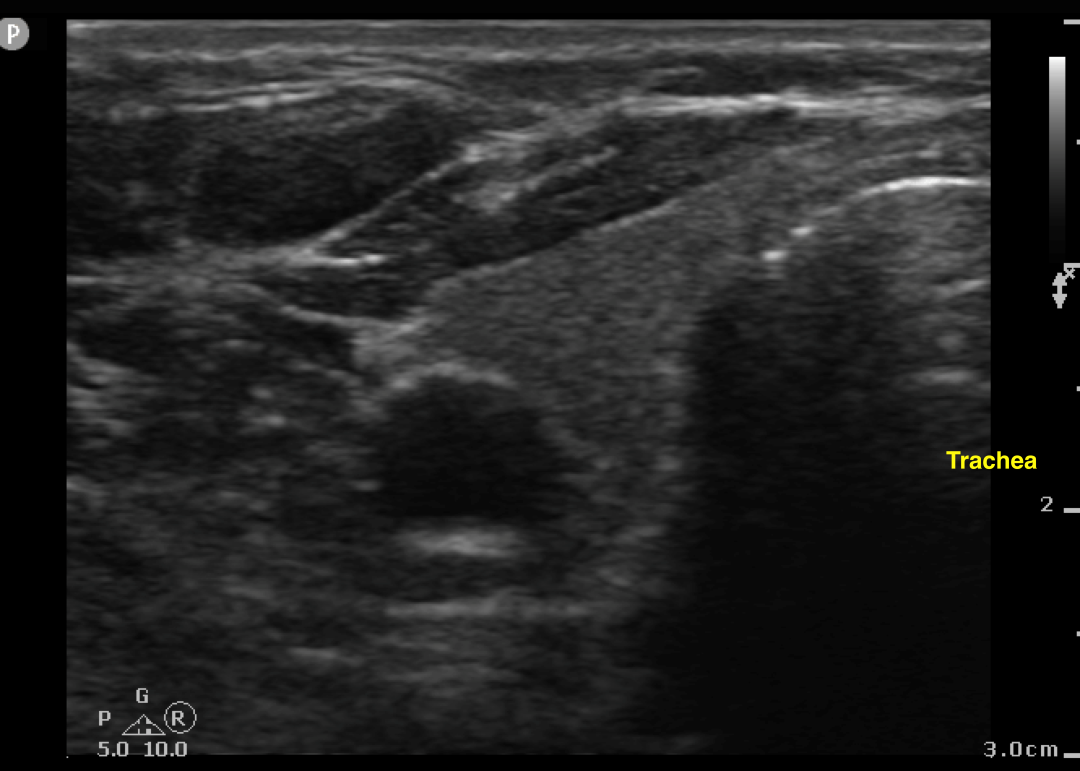
Fig. 3: Bisected trachea, transverse plane, at the level of the sternal notch.
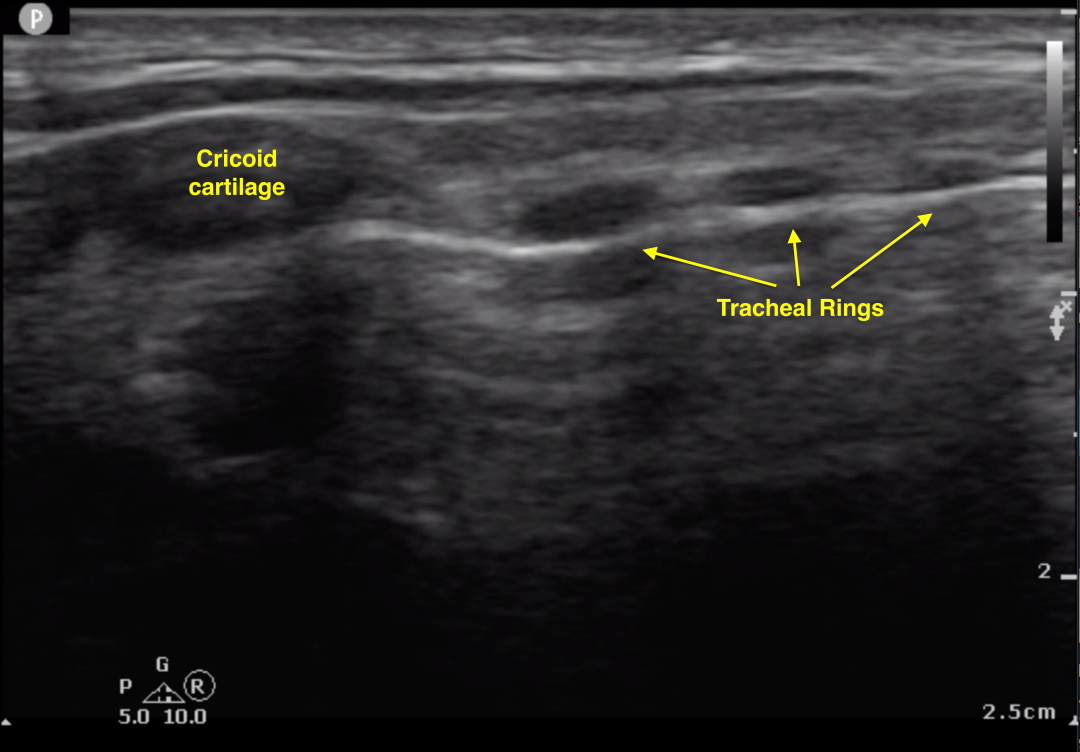
Fig. 4: Trachea, longitudinal plane – tracheal rings/string of pearls.
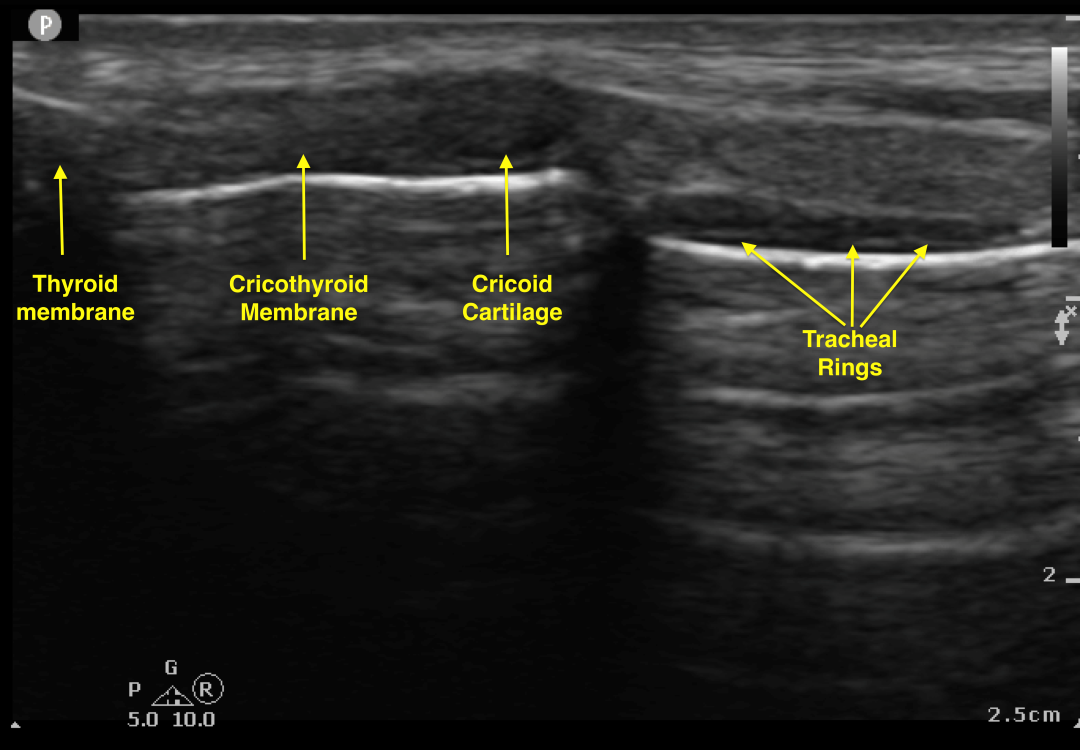
Fig. 5: Trachea, longitudinal plane – cricoid, thyroid and cricothyroid membrane.
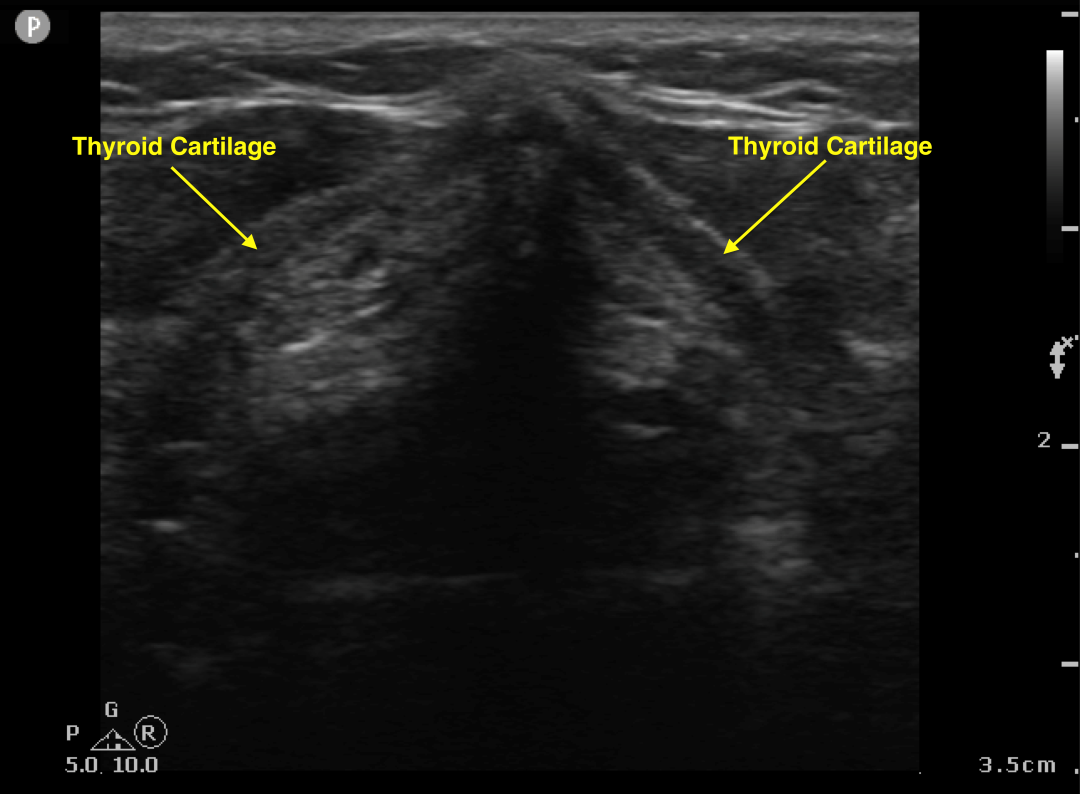
Fig. 6: Thyroid cartilage, transverse plane.
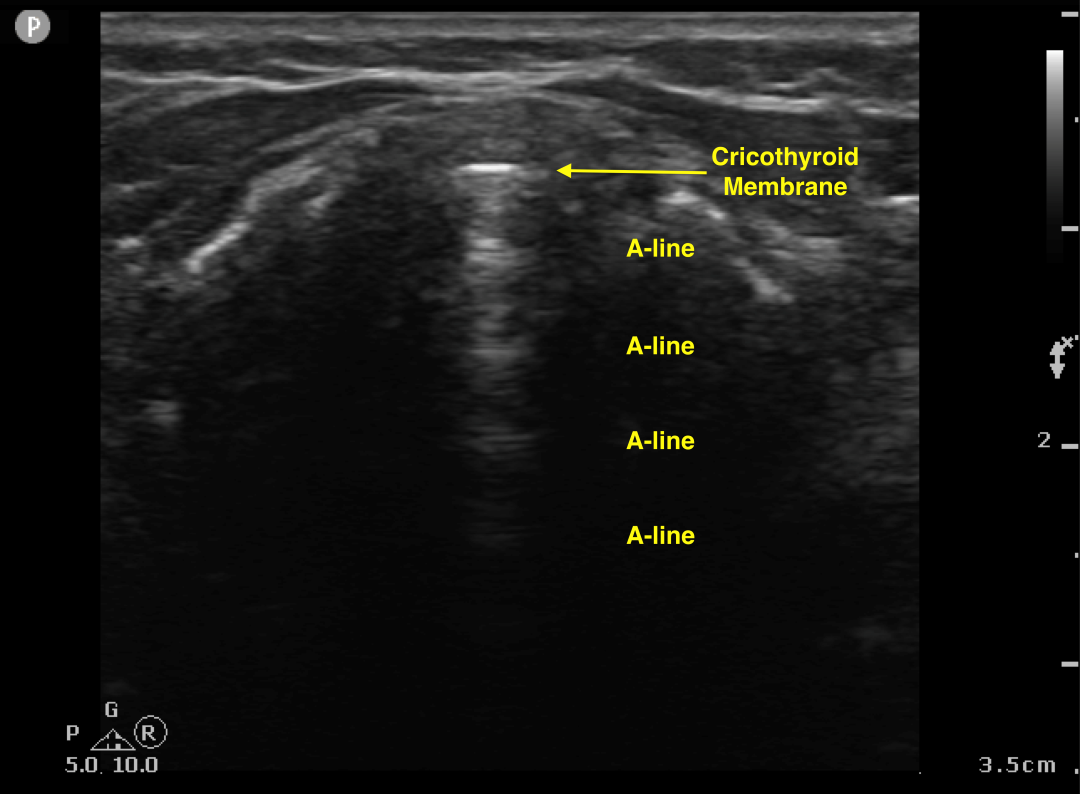
Fig. 7: Cricothryoid membrane, transverse plane.
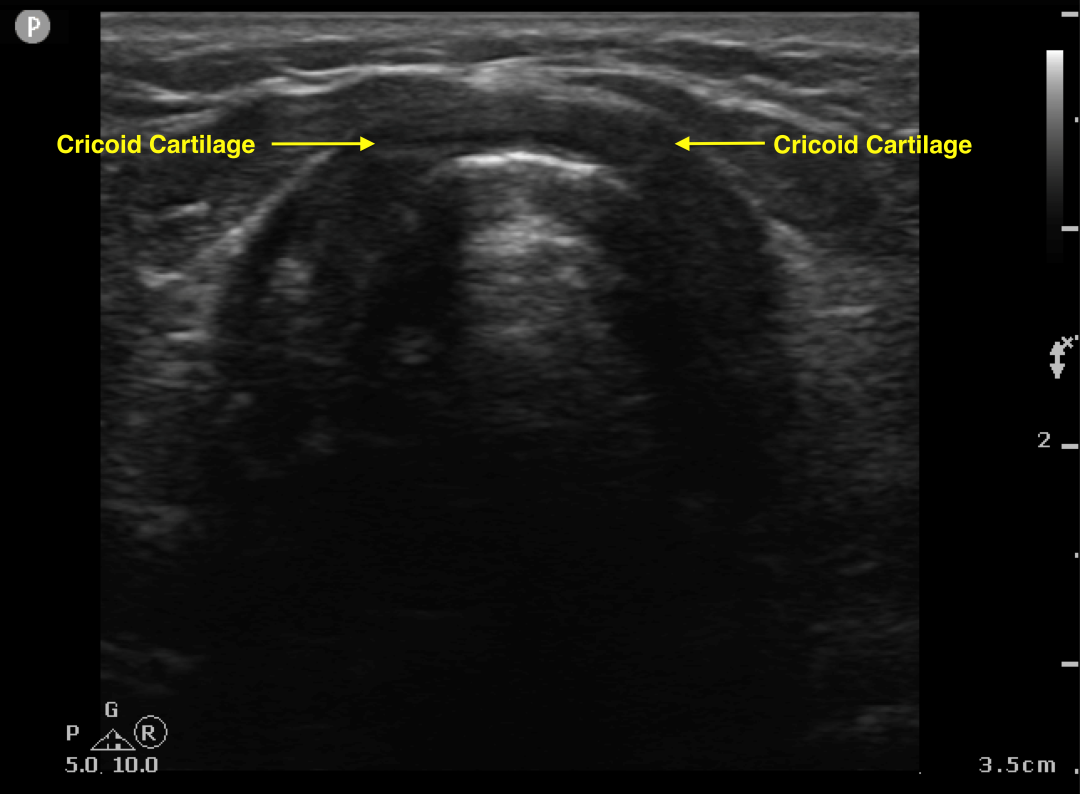
Fig. 8: Cricoid cartilage, transverse plane.
References:
- Gottlieb M, Holladay D, Peksa GD. Ultrasonography for the Confirmation of Endotracheal Tube Intubation: A Systematic Review and Meta-Analysis. Ann Emerg Med. 2018 Dec;72(6):627-636. doi: 10.1016/j.annemergmed.2018.06.024. Epub 2018 Aug 14. PMID: 30119943.
- Mishra PR, Bhoi S, Sinha TP. Integration of Point-of-care Ultrasound during Rapid Sequence Intubation in Trauma Resuscitation. J Emerg Trauma Shock. 2018 Apr-Jun;11(2):92-97. doi: 10.4103/JETS.JETS_56_17. PMID: 29937637; PMCID: PMC5994849.
- Gottlieb M, Holladay D, Burns KM, Nakitende D, Bailitz J. Ultrasound for airway management: An evidence-based review for the emergency clinician. Am J Emerg Med. 2020 May;38(5):1007-1013. doi: 10.1016/j.ajem.2019.12.019. Epub 2019 Dec 11. PMID: 31843325.
- Chou HC, et. al. Tracheal rapid ultrasound exam (T.R.U.E.) for confirming endotracheal tube placement during emergency intubation. Resuscitation. 2011 Oct;82(10):1279-84. doi: 10.1016/j.resuscitation.2011.05.016. Epub 2011 Jun 1. PMID: 21684668.
- Sahu AK, Bhoi S, Aggarwal P, Mathew R, Nayer J, T AV, Mishra PR, Sinha TP. Endotracheal Tube Placement Confirmation by Ultrasonography: A Systematic Review and Meta-Analysis of more than 2500 Patients. J Emerg Med. 2020 Aug;59(2):254-264. doi: 10.1016/j.jemermed.2020.04.040. Epub 2020 Jun 14. PMID: 32553512.
- Alerhand S. Ultrasound for identifying the cricothyroid membrane prior to the anticipated difficult airway. Am J Emerg Med. 2018 Nov;36(11):2078-2084. doi: 10.1016/j.ajem.2018.07.027. Epub 2018 Jul 12. PMID: 30025948.
This article is part of the following sections: