The Impact of Covid-19 on Influenza Incidence at a Community Hospital
Since its emergence in late 2019, severe acute respiratory syndrome coronavirus 2 (COVID-19) has been compared with endemic influenza (Stowe et al., 2021; Chotpitayasunondh et al., 2020; Belingheri et al., 2020; Belongia et al., 2020: Iacobucci et al. 2020). These viruses share important similarities, but have distinct differences, as COVID-19 is significantly more infectious and exhibits a greater variety of symptoms (Kiseleva et al., 2021; Rodríguez et al., 2021; Olsen et al., 2021).
Mask mandates and social distancing recommendations have been shown to be effective in reducing COVID-19 and influenza transmission during 2020 (Odone, 2020; Soo et al., 2020; Feng et al., 2021). COVID-19 and influenza data from 2021 and 2022 however, is less studied. This article aims to review and discuss influenza and COVID-19 data from a community hospital in Indian River County from August 2021 to July 2022.
Indian River County followed Florida state mandates throughout the pandemic, and many businesses maintained mask requirements after such restrictions were completely lifted statewide in September 2020 (Lapin et al., 2020; Leake et al., 2022). Indian River County also maintains a higher COVID-19 vaccination rate than the United States average, despite lacking a COVID-19 vaccination mandate. In this county, 87.12% of people have at least one vaccine dose and 73.42% are considered fully vaccinated compared to 79% and 68%, respectively, nationwide (DOT, 2021; USAFacts, 2022).
Emergency Department COVID-19 and influenza data from Sebastian River Medical Center during the period from August 1st, 2021 to July 31, 2022 were used for this analysis. COVID-19 cases are recorded as the combined number of positive COVID-19 PCR and Antigen test data. If a patient received both tests, solely the result of the COVID-19 PCR was recorded. Influenza tests differentiated between A and B variants. Interestingly, during this particular time period, no patient tested positive for both influenza and COVID-19.
Results
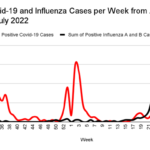
Total new COVID-19 cases per week were increasing throughout July and into August of 2021, peaking at 44 cases per week during week 34 before decreasing. The number of new COVID-19 cases stayed quite low until week 51, when cases increased dramatically, eventually peaking at 60 new COVID-19 cases in week 2 of 2022. The number of new COVID-19 cases then plummeted again until the middle of April (week 15), when the number of cases again started to increase, maintaining a level of approximately 10 new cases a week until the end of the dataset (July) (Figure 1).
Figure 1:
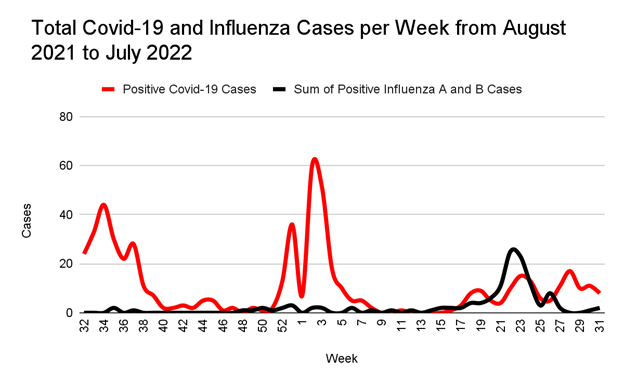
Interestingly, the number of new influenza cases remained virtually nonexistent from week 32 (August 2021) to week 18 (early May 2022). After this, total influenza cases per week began to increase, culminating in a significant increase to 25 cases during week 22. Influenza cases then rapidly declined, despite COVID-19 maintaining a steady rate of about 10 cases per week (Figure 1). It is curious that the peak of influenza in weeks 21 through 25 was nearly all influenza A (Figure 2).
Figure 2:
Discussion
Three distinct peaks of COVID-19 activity occurred in this dataset. The first peak began in early August (week 32). This corresponded with the reopening of schools. Many studies have shown that the reopening of schools was correlated with an increase in COVID-19 transmission (Oster et al., 2021; Atherstone et al., 2021; Siegel et al., 2021; Monod et al. 2021).
The second peak of COVID-19 cases occurred from December 2021 to January 2022. This was during the holiday season, when travel is known to increase and family members travel into the community. It is harder to maintain social distancing while traveling and people may not have the option of staying away from people that are less compliant with masking mandates. Multiple authors believe these factors to play a large part in COVID-19 case spikes (Peacock et al., 2021; Bratić et al., 2021; Mehta et al., 2021; Su et al., 2021).
A third series of peaks in new COVID-19 cases occurred between weeks 16 to 31 (April to August). Multiple theories have been postulated to explain these recurrent moderate spikes in COVID-19 activity. These include the end of the school year and summer travel, the associated increase in influenza (see below), and a significant amount of “COVID fatigue” with people being less cautious with preventative measures (Chen et al., 2021; Joli et al., 2022; Rudroff et al., 2020; Tonzel& Sokol, 2021).
Throughout the 2020 to 2021 influenza season, strict mask mandates were in place across most of the country. People were very cautious about social distancing and hand cleanliness. It is not surprising, therefore, that influenza cases were dramatically lower than normal trends. This was first reported in Australia, where the influenza season is earlier than the season in the United States (Odone, 2020; Soo et al., 2020; Feng et al., 2021).
Perhaps the most curious finding in this dataset is the peak of influenza A cases during the summer of 2022 (week 21 to 25). It is generally believed that viruses, especially influenza, are less able to spread during the summer due to decreased proximity and other factors (Reichert, 2004; Barr, 1990; Simonsen, 2005). The 2021 peak of influenza A cases deviates from normal trends significantly (Reichert, 2004; Barr, 1990; Simonsen, 2005). Before the onset of COVID-19, influenza peaked during the winter months, which is believed to occur due to increased proximity to others (Reichert, 2004; Barr, 1990; Simonsen, 2005). Florida is unique due to the arrival of “snow-birds” from the northern areas of the country during the winter months (Chui et al., 2011). The 2022 flu season peaked during the summer before the arrival of the “snow-birds.” Other studies have also observed this trend (Odone et al., 2020; Soo et al., 2020; Stojanovic et al., 2021; Lee et al., 2020). It may be due to decreased testing or virus-virus interactions, both of which have been documented during the COVID-19 pandemic (Koutsakos et al., 2021; Lee et al., 2020; Hills et al., 2020). However, further research is needed to determine the exact cause of this trend.
Conclusion
The COVID-19 pandemic is a once in a century event with a multifaceted impact on medicine. One of the most interesting impacts is the effect the pandemic had on the incidence of seasonal influenza. The data presented here review the impact of the COVID-19 pandemic on the incidence of influenza during the 2021-2022 season as observed at a community hospital in Indian River County, Florida. A significant decrease in influenza cases is noted during the winter influenza season followed by an unexpected peak in influenza activity in the summer. Various theories are postulated to explain the observed changes, but further research is needed. These observations can play an important role in preparing for future pandemics.
References
- Atherstone, C., Siegel, M., Schmitt-Matzen, E., Sjoblom, S., Jackson, J., Blackmore, C., &Neatherlin, J. (2021). SARS-CoV-2 Transmission Associated with High School Wrestling Tournaments — Florida, December 2020–January 2021. MMWR. Morbidity and Mortality Weekly Report, 70(4), 141–143. https://doi.org/10.15585/mmwr.mm7004e4
- Barr, C. E. (1990). Exposure to Influenza Epidemics During Gestation and Adult Schizophrenia. Archives of General Psychiatry, 47(9), 869. https://doi.org/10.1001/archpsyc.1990.01810210077012
- Belongia, E. A., &Osterholm, M. T. (2020). COVID-19 and flu, a perfect storm. Science, 368(6496), 1163–1163. https://doi.org/10.1126/science.abd2220
- Bratić, M., Radivojević, A., Stojiljković, N., Simović, O., Juvan, E., Lesjak, M., &Podovšovnik, E. (2021). Should I Stay or Should I Go? Tourists’ COVID-19 Risk Perception and Vacation Behavior Shift. Sustainability, 13(6), 3573. https://doi.org/10.3390/su13063573
- Chen, S., Prettner, K., Kuhn, M., Geldsetzer, P., Wang, C., Bärnighausen, T., & Bloom, D. E. (2021). Climate and the spread of COVID-19. Scientific Reports, 11(1). https://doi.org/10.1038/s41598-021-87692-z
- Chui, K. K., Cohen, S. A., & Naumova, E. N. (2011). Snowbirds and infection–new phenomena in pneumonia and influenza hospitalizations from winter migration of older adults: A spatiotemporal analysis. BMC Public Health, 11(1). https://doi.org/10.1186/1471-2458-11-444
- DOT. (2022). Springfield COVID-19 Vaccine Tracker. Springfield News-Leader. https://data.news-leader.com/covid-19-vaccine-tracker/
- Feng, L., Zhang, T., Wang, Q., Xie, Y., Peng, Z., Zheng, J., Qin, Y., Zhang, M., Lai, S., Wang, D., Feng, Z., Li, Z., & Gao, G. F. (2021). Impact of COVID-19 outbreaks and interventions on influenza in China and the United States. Nature Communications, 12(1). https://doi.org/10.1038/s41467-021-23440-1
- Hills, T., Kearns, N., Kearns, C., & Beasley, R. (2020). Influenza control during the COVID-19 pandemic. The Lancet, 396(10263), 1633–1634. https://doi.org/10.1016/s0140-6736(20)32166-8
- Iacobucci, G. (2020). Covid-19: Risk of death more than doubled in people who also had flu, English data show. BMJ, m3720. https://doi.org/10.1136/bmj.m3720
- Joli, J., Buck, P., Zipfel, S., & Stengel, A. (2022). Post-COVID-19 fatigue: A systematic review. Frontiers in Psychiatry, 13. https://doi.org/10.3389/fpsyt.2022.947973
- Kiseleva, I., &Ksenafontov, A. (2021). COVID-19 Shuts Doors to Flu but Keeps Them Open to Rhinoviruses. Biology, 10(8), 733.
- https://doi.org/10.3390/biology10080733
- Koutsakos, M., Wheatley, A. K., Laurie, K., Kent, S. J., & Rockman, S. (2021). Influenza lineage extinction during the COVID-19 pandemic? Nature Reviews Microbiology, 19(12), 741–742.https://doi.org/10.1038/s41579-021-00642-4
- Lapin, T. (2020, March 2). Florida declares public health emergency after two coronavirus cases. New York Post; New York Post. https://nypost.com/2020/03/02/florida-declares-public-health-emergency-after-two-coronavirus-cases/
- Lee, H., Lee, H., Song, K.-H., Kim, E. S., Park, J. S., Jung, J., Ahn, S., Jeong, E. K., Park, H., & Kim, H. B. (2020). Impact of Public Health Interventions on Seasonal Influenza Activity During the COVID-19 Outbreak in Korea. Clinical Infectious Diseases. https://doi.org/10.1093/cid/ciaa672
- Mehta, S. H., Clipman, S. J., Wesolowski, A., & Solomon, S. S. (2021). Holiday gatherings, mobility and SARS-CoV-2 transmission: results from 10 US states following Thanksgiving. Scientific Reports, 11(1). https://doi.org/10.1038/s41598-021-96779-6
- Monod, M., Blenkinsop, A., Xi, X., Hebert, D., Bershan, S., Tietze, S., Baguelin, M., Bradley, V. C., Chen, Y., Coupland, H., Filippi, S., Ish-Horowicz, J., McManus, M., Mellan, T., Gandy, A., Hutchinson, M., Unwin, H. J. T., van Elsland, S. L., Vollmer, M. A. C., & Weber, S. (2021). Age groups that sustain resurging COVID-19 epidemics in the United States. Science, 371(6536). https://doi.org/10.1126/science.abe8372
- Odone, A., Bucci, D., Croci, R., Riccò, M., Affanni, P., & Signorelli, C. (2020). Acta Biomed, 91, 2020031. https://doi.org/10.23750/abm.v91i3.10549
- Olsen, S. J., Winn, A. K., Budd, A. P., Prill, M. M., Steel, J., Midgley, C. M., Kniss, K., Burns, E., Rowe, T., Foust, A., Jasso, G., Merced-Morales, A., Davis, C. T., Jang, Y., Jones, J., Daly, P., Gubareva, L., Barnes, J., Kondor, R., & Sessions, W. (2021). Changes in Influenza and Other Respiratory Virus Activity During the COVID-19 Pandemic — United States, 2020–2021. MMWR. Morbidity and Mortality Weekly Report, 70(29), 1013–1019. https://doi.org/10.15585/mmwr.mm7029a1
- Oster, E., Jack, R., Halloran, C., Schoof, J., & McLeod, D. (2021). COVID-19 Mitigation Practices and COVID-19 Rates in Schools: Report on Data from Florida, New York and Massachusetts. https://doi.org/10.1101/2021.05.19.21257467
- Peacock, J. E., Herrington, D. M., Edelstein, S. L., Seals, A. L., Plumb, I. D., Saydah, S., Lagarde, W. H., Runyon, M. S., Maguire, P. D., Correa, A., Weintraub, W. S., Wierzba, T. F., Sanders, J. W., Walton, J., Espeland, M. A., Mongraw-Chaffin, M., Bertoni, A., Alexander-Miller, M. A., Mathews, A., & Munawar, I. (2021). Survey of Adherence with COVID-19 Prevention Behaviors During the 2020 Thanksgiving and Winter Holidays Among Members of the COVID-19 Community Research Partnership. Journal of Community Health, 47(1), 71–78. https://doi.org/10.1007/s10900-021-01021-z
- Reichert, T. A. (2004). Influenza and the Winter Increase in Mortality in the United States, 1959-1999. American Journal of Epidemiology, 160(5), 492–502. https://doi.org/10.1093/aje/kwh227
- Rodriguez, A., Nikhil Muralidhar, Adhikari, B., & B. Aditya Prakash. (2020, September 23). Steering a Historical Disease Forecasting Model Under a Pandemic: Case of Flu and COVID-19. ResearchGate; unknown. https://www.researchgate.net/publication/344373541_Steering_a_Historical_Disease_Forecasting_Model_Under_a_Pandemic_Case_of_Flu_and_COVID-19
- Rough, J. (2022, November). What to Say When A Household Member Won’t Get Vaccinated. AARP.
- https://www.aarp.org/politics-society/government-elections/info-2020/coronavirus-state-restrictions.html
- Rudroff, T., Fietsam, A. C., Deters, J. R., Bryant, A. D., &Kamholz, J. (2020). Post-COVID-19 Fatigue: Potential Contributing Factors. Brain Sciences, 10(12), 1012. https://doi.org/10.3390/brainsci10121012
- Siegel, M., Kloppenburg, B., Woerle, S., Sjoblom, S., &Danyluk, G. (2021). Notes from the Field: SARS-CoV-2 Transmission Associated with High School Football Team Members — Florida, September–October 2020. MMWR. Morbidity and Mortality Weekly Report, 70(11), 402–404. https://doi.org/10.15585/mmwr.mm7011a3
- Simonsen, L., Reichert, T., Viboud, C., Blackwelder, W., Taylor, R., & Miller, M. (2005). Impact of Influenza Vaccination on Seasonal Mortality in the US Elderly Population. Archives of Internal Medicine, 165(3), 265. https://doi.org/10.1001/archinte.165.3.265
- Soo, R. J. J., Chiew, C. J., Ma, S., Pung, R., & Lee, V. (2020). Decreased Influenza Incidence under COVID-19 Control Measures, Singapore. Emerging Infectious Diseases, 26(8), 1933–1935. https://doi.org/10.3201/eid2608.201229
- Stojanovic, J., Boucher, V. G., Boyle, J., Enticott, J., Lavoie, K. L., & Bacon, S. L. (2021). COVID-19 Is Not the Flu: Four Graphs From Four Countries. Frontiers in Public Health, 9. https://doi.org/10.3389/fpubh.2021.628479
- Stowe, J., Tessier, E., Zhao, H., Guy, R., Muller-Pebody, B., Zambon, M., Andrews, N., Ramsay, M., & Lopez Bernal, J. (2021). Interactions between SARS-CoV-2 and influenza, and the impact of coinfection on disease severity: a test-negative design. International Journal of Epidemiology, 50(4), 1124–1133. https://doi.org/10.1093/ije/dyab081
- Su, Z., Wen, J., McDonnell, D., Goh, E., Li, X., Šegalo, S., Ahmad, J., Cheshmehzangi, A., & Xiang, Y.-T. (2021). Vaccines are not yet a silver bullet: The imperative of continued communication about the importance of COVID-19 safety measures. Brain, Behavior, & Immunity – Health, 12, 100204. https://doi.org/10.1016/j.bbih.2021.100204
- Tonzel, J. L., & Sokol, T. (2021). COVID-19 Outbreaks at Youth Summer Camps — Louisiana, June–July 2021. MMWR. Morbidity and Mortality Weekly Report, 70(40), 1425–1426. https://doi.org/10.15585/mmwr.mm7040e2
- USAFacts. (2022, December 9). US Coronavirus vaccine tracker. USAFacts; USAFacts. https://usafacts.org/visualizations/covid-vaccine-tracker-states
This article is part of the following sections: