Going to the Beach to Catch the Peaked T-Waves: Heat Stroke Causing Multiorgan Failure
Introduction
An undifferentiated, unresponsive patient provides a unique challenge in the emergency department. We present a case of a patient with heat stroke after polysubstance use, who was found to have rhabdomyolysis, severe hyperkalemia, and multiple organ failure.Case
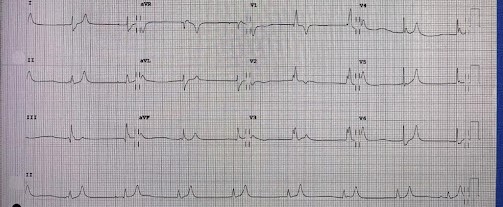
A 59-year-old male was brought by EMS after he was found unresponsive at the beach. EMS states that he had not moved for seven hours and that bottles of alcohol and two small bags of drugs were found at the scene. For EMS, the patient’s glucose was 36. They gave him one ampule of dextrose 50% and naloxone, which did not improve his mental status. When the patient arrived at the ED, his core temperature was 39.2 degrees celsius with systolic blood pressures in the 90s, and a GCS of 7 (eyes open, incomprehensible sounds, no motor response). On the monitor, the patient had bouts of irregular tachycardia and bradycardia with erratic PVCs and couplets. The EKG demonstrated bradycardia with peaked T-waves (Figure 1). Upon conducting a physical exam, the patient had diffuse erythema and ~10% body surface area was covered by bullae on his legs, back, buttocks, and groin (Figure 2). The patient’s initial labs were significant for: potassium 7.2; creatine 4.04; high sensitivity troponin 293; arterial blood gas pH 7.22, PCO2 46.9, HCO3 18.7; WBC 16.9; positive for MDMA, benzodiazepines, and marijuana; total creatine kinase 10,980; ammonia 206; total bilirubin 3.8; AST 23,440; ALT 6370; and Lactic Acid 5.2. CT brain did not demonstrate any acute findings.Given the patient’s severely decreased mental status, he was intubated using etomidate and rocuronium. Based upon the initial EKG and arrhythmias noted on the monitor, the patient was empirically given four liter boluses of normal saline, six grams of calcium gluconate, four ampules of sodium bicarbonate, and 10 units of intravenous insulin with one ampule of dextrose 50% repeated three times. After receiving this regimen, the patient was in normal sinus rhythm with a repeat potassium of 5.4. After fluid resuscitation, he had only 400 mL of urine output and remained hypotensive, requiring a norepinephrine drip. A dialysis catheter was placed in the ER to facilitate emergent initiation of renal replacement therapy upon ICU admission. Eleven days after initial presentation, treatment was determined futile and care was withdrawn.
Discussion
This is a case of an unresponsive patient suffering from heat stroke associated with polysubstance intoxication. Given that the outdoor temperature was 90 degrees Fahrenheit, the patient’s use of MDMA may have contributed to his hyperthermia. Secondarily, the patient developed rhabdomyolysis, hyperkalemia, circulatory failure, acute liver failure, acute renal failure, and metabolic encephalopathy.
Heat stroke is a severe heat-related illness resulting in an acute increase in core body temperature and a decreased mental status. Early recognition and treatment of heat stroke is often challenging given how similar the presentation is to sepsis, drug overdose, and stroke. One study found that of 3,372 hospitalizations for heatstroke, 12% of the patient developed shock and these patients had a 7.1-times higher mortality rate. [1]
The same group published another study where the mortality rate of patients with heatstroke was 5%, 20% required intubation, 2% required renal replacement therapy, and rhabdomyolysis was the most common complication of heat stroke. [2] The most common systems of end-organ failure were renal, followed by neurological, respiratory, metabolic, hematologic, circulatory, and liver. [2] Both rhabdomyolysis and acute kidney injury occurred in roughly a third of heat stroke patients and were associated with increased morbidity and mortality in these patients. [3,4] The patient in our case presented with many of the complications of heat stroke that are typically encountered during a hospital course and not upon arrival. The aggressive use of intravenous fluids in our case played two roles: it helped to cool the patient, while simultaneously treating his acute kidney failure and rhabdomyolysis.
Another important aspect of this case was the patient’s severe hyperkalemia, which was suspected from the erratic arrhythmias on the patient’s monitor and EKG. These arrhythmias allowed us to rapidly and aggressively treat this patient’s hyperkalemia and prevent the patient from going into cardiac arrest. Despite being a common presentation to the emergency department, there is not one standardized treatment for hyperkalemia, although it typically involves stabilizing the cardiac membrane, shifting potassium back into the cells, and removing potassium from the body. Both calcium gluconate and calcium chloride have a rapid onset of action, a duration of action of about 30-50 minutes, and can be frequently re-administered to stabilize the cardiac membrane, if EKG changes persist. [5] The administration of regular intravenous insulin acts to shift potassium into the cells, has a peak effect within 30 minutes, and has a duration of action of two to four hours. [5] Second-line potassium shifting medications include sodium bicarbonate, which has only been effective in the setting of metabolic acidosis, and 20mg of nebulized albuterol, which has a peak effect within 30 minutes and a duration of action between two and six hours. [5] In patients with functioning kidneys, furosemide can be particularly effective at removing excess potassium in fluid overloaded patients, with an onset of action of 30 to 60 minutes. Aggressive use of intravenous fluids in patients who are volume depleted can help dilute the potassium concentration. [5] In cases of severe hyperkalemia or new renal failure, early insertion of a dialysis catheter in the emergency department facilitates earlier initiation of continuous renal replacement therapy or hemodialysis.
The three most important teaching points from this case are: 1) Heat stroke should be high on your differential even in non-exertional cases, as rapid identification and cooling are important for reducing morbidity and mortality; 2) Early identification and aggressive treatment of hyperkalemia based upon monitor or EKG changes before a potassium level is resulted can prevent cardiac arrest; and 3) Be aware of the complications of heat stroke and identify and treat them on initial presentation. ■
References
- Bathini T, Thongprayoon C, Petnak T, et al. Circulatory Failure among Hospitalizations for Heatstroke in the United States. Medicines (Basel). 2020;7(6):32. Published 2020 Jun 14. doi:10.3390/medicines7060032
- Kaewput W, Thongprayoon C, Petnak T, et al. Inpatient burden and mortality of heatstroke in the United States. Int J Clin Pract. 2021;75(4):e13837. doi:10.1111/ijcp.13837
- Thongprayoon C, Petnak T, Kanduri SR, et al. Impact of rhabdomyolysis on outcomes of hospitalizations for heat stroke in the United States. Hosp Pract (1995). 2020;48(5):276-281. doi:10.1080/21548331.2020.1792214
- Thongprayoon C, Qureshi F, Petnak T, et al. Impact of Acute Kidney Injury on Outcomes of Hospitalizations for Heat Stroke in the United States. Diseases. 2020;8(3):28. Published 2020 Jul 15. doi:10.3390/diseases8030028
- Lasure Ben, Shaver Erica. Hyperkalemia. In: Mattu A and Swadron S, ed. CorePendium. Burbank, CA: CorePendium, LLC. emrap.org/corependium/chapter/recEcOnShorJunqD5/Hyperkalemia#h.3siw3n2u4xbv. Updated July 6, 2021. Accessed September 22, 2022.
This article is part of the following sections: