Successful Treatment of Massive Pulmonary Embolism in Pregnancy with Catheter-Directed Embolectomy
Introduction:
Currently there are no treatment guidelines for massive pulmonary embolism (PE) in pregnancy and limited data exist to help guide treatment strategies. Catheter-directed embolectomy can be a viable consideration and offers the benefit of decreased maternal bleeding associated with thrombolysis. (3)
Case:
A 37-year-old female with bipolar disorder, anemia, endometriosis, and obesity presented to the emergency department by ambulance for chest pain, shortness of breath that precluded a syncopal episode. Paramedics placed the patient on nasal cannula and non-rebreather for profound hypoxia and noted the patient to be hypotensive enroute. On arrival, the patient is normotensive, tachycardic and hypoxic and placed on BiPAP. EKG (Figure 1) showed S1Q3T3 pattern, ST segment depression in lateral leads and incomplete RBBB. Patient was started on heparin drip empirically. CTA of the chest (Figure 2) showed occlusive bilateral PE beginning at the first bifurcation of the bilateral pulmonary arteries, evidence of right heart strain, and evidence of possible intrauterine pregnancy. Subsequent b-HCG was positive, and after discussion with interventional cardiology and patient, she was taken for emergent catheter-directed embolectomy (Figure 3). The patient’s condition immediately improved after thrombectomy with heart rate decreasing from 135 to 99 and oxygen requirement declining to 2L/min NC. The patient was continued on anticoagulation and her hypercoagulation workup was negative. Pelvic ultrasound performed later confirmed a viable intrauterine pregnancy estimated at 10 weeks gestation. She was discharged after 4 days with therapeutic Lovenox and follow-up with high-risk OB and hematology.
Discussion:
Pregnant patients are at increased risk of blood clots due to venous stasis and hypercoagulability ultimately leading to PE being the leading cause of maternal mortality. (1) Massive PE in pregnancy has been associated with a mortality rate as high as 37%.(2) Treatment for massive PE in non-pregnant patients is initially with systemic thrombolysis due to reported mortality benefit. However, pregnant patients have been excluded from clinical trials and no controlled studies have been performed(1).
Although pregnancy is considered a relative contraindication for thrombolysis, limited alternative options force its consideration.(1) Embolectomy via percutaneous or surgical approach are also reasonable options, especially to avoid the bleeding risk associated with thrombolysis. (2)
While thrombolytics can take hours for clinical improvement to be appreciated, patients who undergo catheter-directed embolectomy have shown rapid improvement.(2) Catheter-directed embolectomy is not without its limitations including limited facilities with the appropriate equipment and staff to perform the procedure. As well as complications that include clot fragmentation, vessel damage and pulmonary arterial dissection. Despite these limitations and risks, catheter-based embolectomy can be considered as an initial treatment option in the pregnant population in which thrombolytics and surgical thrombectomy place significant risk and complications for both the mother and fetus.
Conclusion:
As demonstrated by our case, we endorse that catheter-directed embolectomy in pregnant patients who present with a massive PE is a viable initial treatment option.
References
- Heavner, M.S., Zhang, M., Bast, C.E., Parker, L. and Eyler, R.F. (2017). Thrombolysis for Massive Pulmonary Embolism in Pregnancy. Pharmacotherapy, 37: 1449-1457. https://doi.org/10.1002/phar.2025
- Hobohm, L., Farmakis, I. T., Münzel, T., Konstantinides, S., & Keller, K. (2022). Pulmonary embolism and pregnancy—challenges in diagnostic and therapeutic decisions in high-risk patients. Frontiers in Cardiovascular Medicine, 9. https://doi.org/10.3389/fcvm.2022.856594
- Martillotti, G., Boehlen, F., Robert‐Ebadi, H., Jastrow, N., Righini, M., & Blondon, M. (2017). Treatment options for severe pulmonary embolism during pregnancy and the postpartum period: A systematic review. Journal of Thrombosis and Haemostasis, 15(10), 1942–1950. https://doi.org/10.1111/jth.13802
- Yarusi, B. B., Jagadeesan, V. S., & Schimmel, D. R. (2020). Not for the faint of heart. Circulation, 142(5), 501–506. https://doi.org/10.1161/circulationaha.120.046795
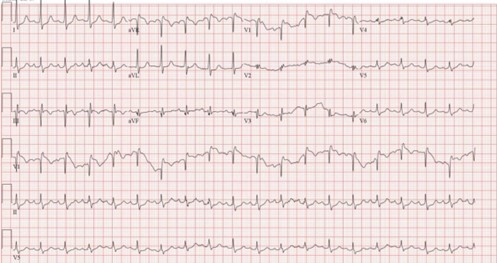
Figure 1
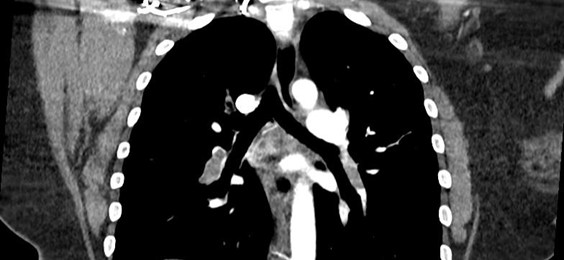
Figure 2
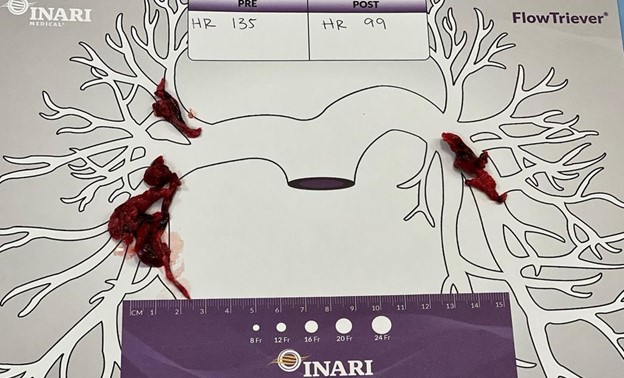
Figure 3
This article is part of the following sections: