Heart Attacks in the Younger Population: A Case of Spontaneous Coronary Artery Dissection
The Case
A 37-year-old female, G1P1 and one week postpartum via C-section, was brought to the emergency department by EMS after having a near-syncopal event at home. The patient reported she was feeding her newborn when she suddenly felt lightheaded and almost passed out. She also endorsed experiencing chest pain, lower back pain and dyspnea. Per the patient, her pregnancy was only notable for in-vitro fertilization during which she was on high-dose hormonal therapy, thrombocytopenia of unknown etiology, and C-section delivery due to thrombocytopenia. Patient denied other symptoms, including abdominal pain or abnormal vaginal bleeding.
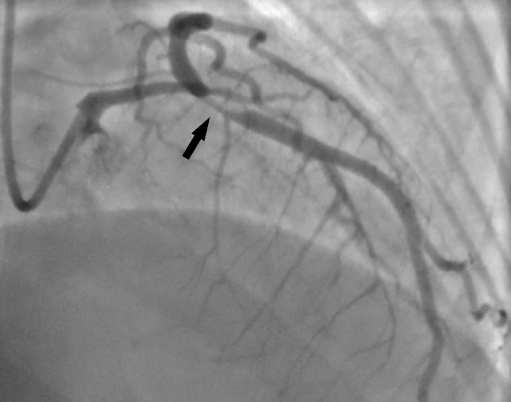
Initial vital signs in the ED showed the patient to be hypotensive (71/53), tachycardic (101 bpm), afebrile (36.3°C), and saturating well (100% on room air). On exam, the patient was noted to be toxic-appearing and in moderate distress. She was also diaphoretic with pale, ashy looking skin and had a delayed capillary refill time. Otherwise, the remaining physical exam was unremarkable. In addition to obtaining labs and starting IV fluids, an immediate electrocardiograph (EKG) was done, which showed diffuse ST depressions with ST elevations in aVR and V1 (see Fig. 1).
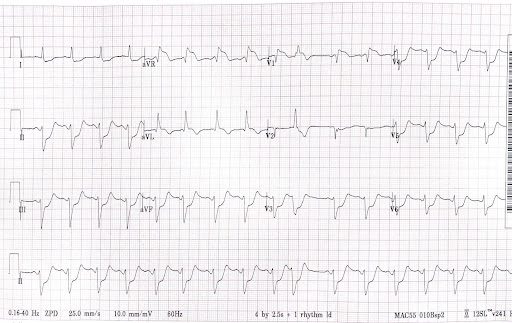
Interventional Cardiology was immediately consulted, and the decision was made to emergently take the patient to the catheterization lab for left heart catheterization. Prior to catheterization, a CT Angio Chest/Abdomen was obtained and negative for pulmonary embolism and aortic dissection. During left heart catheterization, the patient was found to have a coronary artery dissection of the distal left main and proximal left anterior descending arteries (see Fig. 2), consistent with the diagnosis of spontaneous coronary artery dissection.
Diagnosis
Spontaneous coronary artery dissection (SCAD) is a rare spontaneous separation of the coronary arterial wall that can cause acute myocardial infarction. It is estimated that SCAD represents 1-4% of all acute coronary syndrome (ACS) cases. SCAD accounts for nearly 35% of all ACS cases in women less than 50 years old and is the most common cause of myocardial infarctions in patients who are pregnant or postpartum. However, this is likely an underestimate given that many SCAD cases result in sudden cardiac death. It often presents in younger individuals who typically do not have the conventional atherosclerotic risk factors, such as hypertension or diabetes. Some risk factors associated with SCAD include fibromuscular dysplasia, pregnancy, arteriopathies, connective tissue disorders and systemic inflammatory disorders.
Pregnancy-associated SCAD is most often seen during the third trimester and up to six weeks postpartum but can occur at any time during the pregnancy. It also tends to present with more aggressive and extensive dissections compared to non-pregnancy-associated SCAD. While the underlying mechanism of SCAD is poorly understood, it is thought to occur when there is an intimal tear and intramural hematoma formation or spontaneous bleeding of the vasa vasorum leading to narrowing of the coronary artery lumen that subsequently causes myocardial ischemia. In pregnant and postpartum patients, there is a belief that it is due to hormonal changes weakening coronary arterial walls or due to the physiological hemodynamic changes seen in pregnancy, which place increased stress on the coronary arterial walls.
The signs and symptoms seen in SCAD are essentially the same as those seen in an acute myocardial infarction due to atherosclerosis, with chest pain being the most common symptom. Less common symptoms include arm pain, neck pain, back pain, dyspnea, nausea and vomiting. The most common EKG findings are ischemic changes, such as ST elevations affecting the left anterior descending artery and occasionally affecting the left main coronary artery. It is often diagnosed with coronary angiography where a dissection will be visible in the absence of atherosclerosis.
There are a wide range of treatment options, including conservative management, emergency revascularization with percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG), fibrinolytic therapy, mechanical hemodynamic support, and cardiac transplantation. Conservative treatment is preferred in patients with no signs of myocardial ischemia, whereas PCI or CABG is preferred in patients with signs of myocardial ischemia. In cases of SCAD, PCI has a high likelihood of in-stent restenosis, stent mal-apposition, and stent thrombosis. SCAD has an overall mortality rate of over 50%. In patients that survive to hospital admission, the rate of survival to discharge improves to 85%. These patients are typically managed by outpatient cardiology with long-term aspirin, beta-blockers, short-term clopidogrel, and a statin in patients with dyslipidemia.
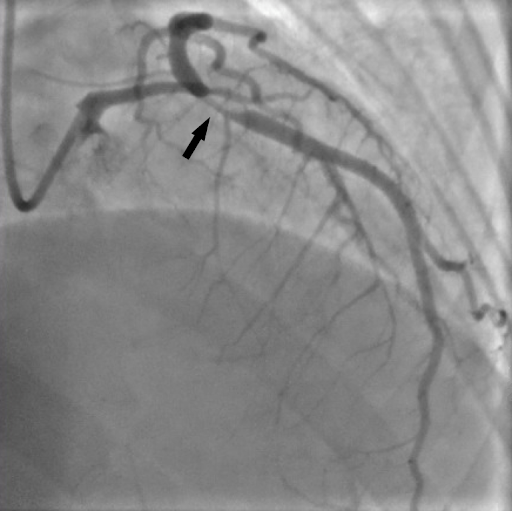
In this patient, two drug-eluting stents were placed (see Fig. 3) along with a right-sided catheter-based miniaturized ventricular assist device due to a reduced ejection fraction of 35-40% in the setting of a high-risk intervention. The patient was subsequently admitted to the ICU where she had an uncomplicated post-catheterization hospital course. She was weaned off the catheter-based miniaturized ventricular assist device after three days and had a repeat echocardiogram demonstrating an improved ejection fraction of 50%. The patient was later discharged from the hospital on dual antiplatelet therapy and has since followed up with the outpatient cardiology team without residual symptoms or complications.
Given the rarity and poor prognosis of this condition, particularly in pregnant and postpartum patients, it is important that emergency physicians consider SCAD when evaluating young, low-risk patients that present to their emergency department with signs and symptoms that are concerning for ACS. ■
References
1. Saw, J. (2021). Spontaneous Coronary Artery Dissection. J.C. Kaski; P.A. Pellikka (Eds.), UpToDate.
2. Kreider, D.; Berberian, J. (2019). STEMI Equivalents: Can’t Miss Patterns, EM Resident.
3. Hayes SN, Kim ESH, Saw J, Adlam D, Arslanian-Engoren C, Economy KE, Ganesh SK, Gulati R, Lindsay ME, Mieres JH, Naderi S, Shah S, Thaler DE, Tweet MS, Wood MJ; on behalf of the American Heart Association Council on Peripheral Vascular Disease; Council on Clinical Cardiology; Council on Cardiovascular and Stroke Nursing; Council on Functional Genomics and Translational Biology; and Stroke Council. Spontaneous coronary artery dissection: current state of the science: a scientific statement from the American Heart Association. Circulation. 2018;137:e523–e557. DOI: 10.1161/CIR.0000000000000564.
4. Arrivi A, Milici C, Bock C, et al. Idiopathic, serial coronary vessels dissection in a young woman with psychological stress: a case report and review of the literature. Case Reports in Vascular Medicine. 2012 ;2012:498465. DOI: 10.1155/2012/498465. PMID: 23133786; PMCID: PMC3485898.
5. Krishnamurthy, M., Desai, R., & Patel, H. (2004). Spontaneous coronary artery dissection in the postpartum period: association with antiphospholipid antibody. Heart (British Cardiac Society), 90(9), e53. doi.org/10.1136/hrt.2004.038869
This article is part of the following sections: