Social Emergency Medicine: Naloxone out of the ED and into the Community
Background
Recent events, including the tragic rash of opioid overdose deaths in Broward County, FL, have highlighted the continued toll that the opioid epidemic has on communities and healthcare systems across the state of Florida. Opioid overdoses remain an epidemic in the United States, and they were responsible for nearly 50,000 deaths in 2019 alone. [1] In that same year, fatal opioid overdoses in Florida increased by 6.5% compared to 2018. [2] However, great strides have been made in the recognition and treatment of opioid use disorder (OUD) over the last decade, due to the tireless efforts of patient advocates. In particular, the increasing distribution and use of naloxone has been one of the most critical interventions in the ongoing opioid epidemic. [3]
Naloxone is a safe, effective opioid antagonist that targets the mu-opioid receptor, displacing exogenous opioid agonists and reversing the life-threatening respiratory depression associated with opioid overdose. [3] In 2015, the Florida Legislature recognized naloxone’s crucial role in combating the opioid epidemic. The ensuing Emergency Treatment for Suspected Opioid Overdose Act (Florida Statutes 381.887) authorized healthcare providers and pharmacists to dispense naloxone to any patient or caregiver who requests it. This law also ensured that a dispensing provider is acting in good faith and exercising reasonable care is granted immunity from civil, criminal or professional liability. [4]
While the distribution of naloxone to first responders (police, emergency medical technicians, and paramedics) has become widespread, initiatives to distribute naloxone directly to members of at-risk communities has been confined to a far narrower subset of populations. [5] In this article, we report on the first emergency department-partnered program in the state of Florida to distribute naloxone directly to the community.
Existing Interventions
Within the South Florida region, naloxone distribution sites can be found at CVS, Walgreens, and through the isavefl.com website. The availability of adequate user training, as well as the cost of this life-saving medication, varies with each vendor. Some community clinics, such as the University of Miami’s IDEA Needle Exchange Clinic, provide both the medication and the proper training for free. However, patients must seek out these clinics to procure this lifesaving medication. Therefore, there is a growing need for more robust community-centered interventions, focusing on naloxone education and distribution to high-risk patients.
Objectives
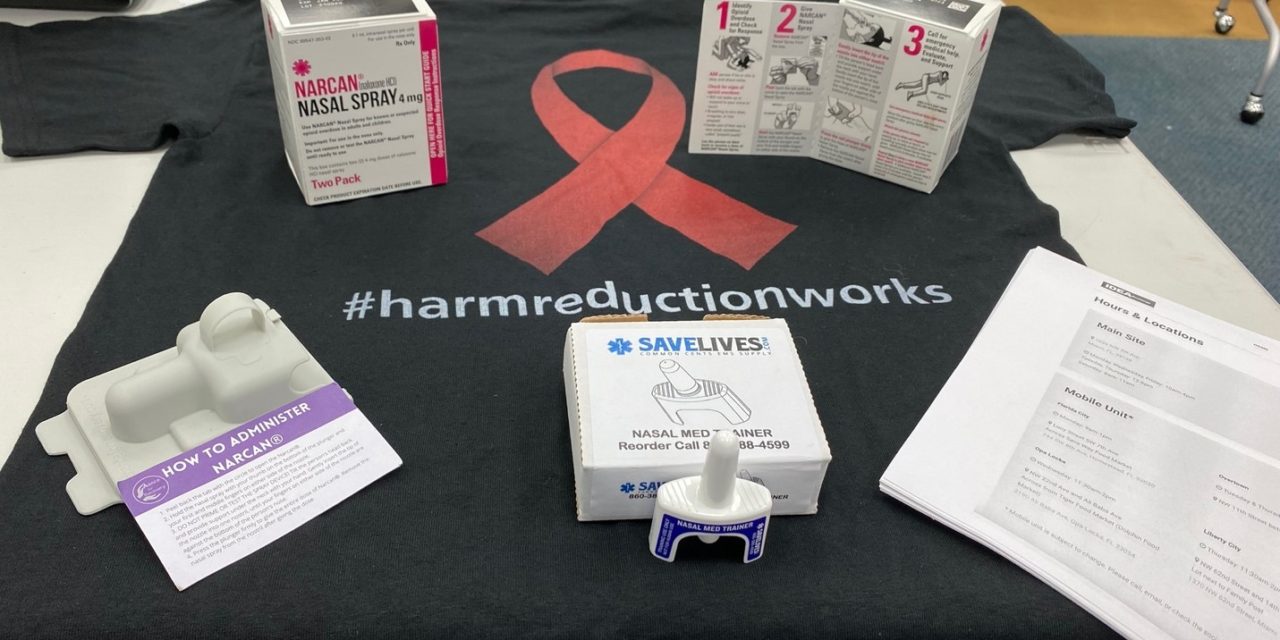
To address South Florida’s opioid epidemic, we aimed to design and implement a novel model for OUD screening and naloxone distribution within the setting of publicly available health fairs. In addition, our group aimed to educate community members on the proper recognition of a suspected opioid overdose and administration of intra-nasal naloxone (commonly known by its brand name, Narcan).
This article highlights our novel model for distribution of naloxone in a community setting at the University of Miami’s medical student-run health fairs. These fairs take place directly in high-risk communities within public spaces, such as churches, schools and community centers. These fairs help providers raise a greater awareness of naloxone across a broader and more varied patient population. These fairs also allow providers to screen for OUD in the community and subsequently distribute naloxone to patients at risk for opioid overdoses.
Methods
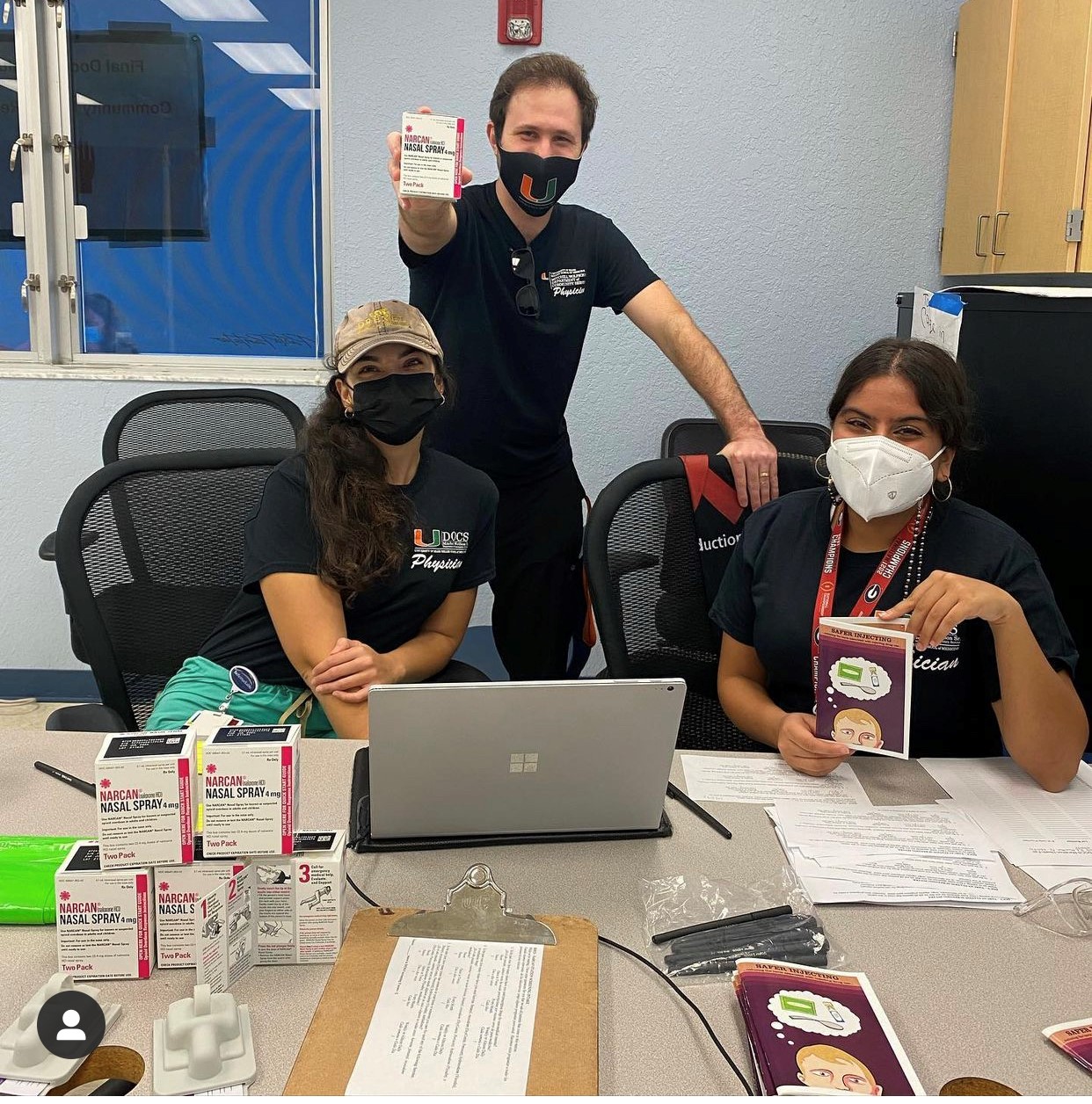
A partnership was established between the University of Miami IDEA Needle Exchange Clinic and the University of Miami Michael Wolfson Department of Community Service (DOCS) program. Patients were screened for OUD by a DOCS Health Fair Screening Volunteer using DSM-5 criteria. [6] All patients who indicated that they, or a member of their household, were at risk for life-threatening opioid overdose were offered naloxone. Naloxone was dispensed by an IDEA Clinic provider, acting under the State of Florida Department of Health Statewide Standing Order For Naloxone (Section 381.887, Florida Statutes). [4]
Implementation and Results
All patients triaged to receive HIV/HCV point-of-care testing at the health fairs were first screened for OUD and offered intra-nasal naloxone (Fig. 1). Patients were provided a sheet of paper with three initial screening questions:
- In the past year, how many times have you used prescription drugs for non-medical reasons?
- In the past year, how many times have you used heroine, fentanyl, oxycodone (OxyContin, Percocet), hydrocodone (Vicodin), or methadone drugs?
- In the past year, how many times has someone in your home or someone you care for used any of the following: heroine, fentanyl, oxycodone (OxyContin, Percocet), hydrocodone (Vicodin), methadone?
Each question had the following options and corresponding points: Never (0), Once or Twice (1), Monthly (2), Weekly/Daily/Almost Daily (3).
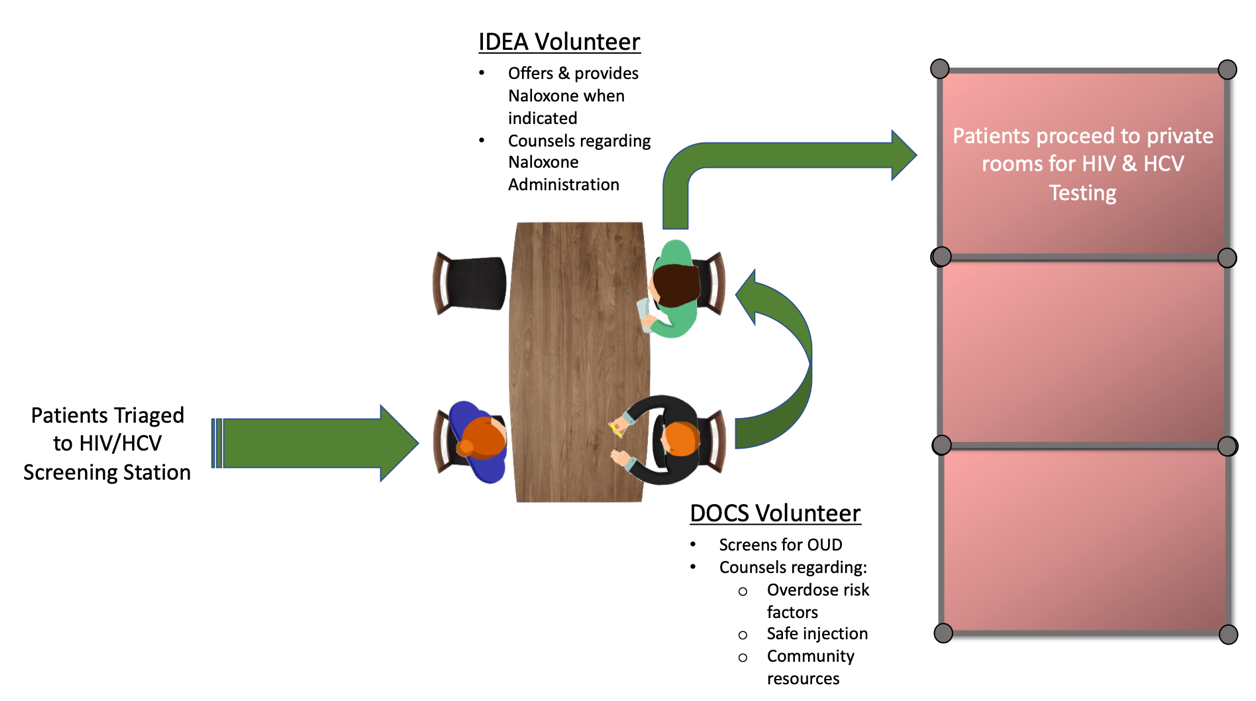
Fig. 1: Schematic of progression of patients undergoing OUD screening and Naloxone education prior to HIV/HCV point-of-care testing.
Responses were recorded in the health fair’s EMR program. Patients who scored a 2 or higher were flagged. Once the flagged patients were in a private space for their HIV/HCV testing, they underwent a more comprehensive screening for OUD, based on the full DSM-5 criteria. Naloxone education was provided to all patients, regardless of their screening scores, to ensure that all patients were aware of the medication’s purpose.
Naloxone was offered to patients who were deemed high-risk after screening, and to any patient who felt they or someone in their household was at risk. Pre-packaged kits, which contain two doses of intranasal naloxone along with pictorial and written instructions, were dispensed. Patients were trained on the indications for use and proper administration, using a “Dummy-Dose” Intranasal Naloxone trainer. Screening questionnaires and administration instructions were printed in English and Spanish. Responses to the OUD screening questions did not affect the patient’s ability to receive HIV/HCV testing. Each distribution site was staffed by an emergency medicine physician. To date, over 200 patients [BK1] have been successfully screened for OUD, and 83 units of naloxone have been dispensed across four health fair sites.
Conclusion
The opioid epidemic continues to affect the state of Florida. OUD screening and education in the community is imperative for better prevention of lethal opioid overdoses. Our team continues to work to decrease the morbidity and mortality associated with OUD, by increasing access to lifesaving naloxone and enhancing communities’ awareness of OUD. We hope that this article will help stimulate the establishment of similar programs elsewhere in Florida. ■
References
- “Drug Overdose Deaths.” Centers for Disease Control and Prevention, Centers for Disease Control and Prevention, 3 Mar. 2021.
- “2020 Overdose Prevention Investment Snapshot – Florida.” 2020 Overdose Prevention Investment Snapshot, Centers for Disease Control & Prevention; National Center for Injury Prevention & Control, 2020.
- Ashton, H. “Intranasal Naloxone in Suspected Opioid Overdose.” Emergency Medicine Journal, vol. 23, no. 3, 2006, pp. 221–223. doi.org/10.1136/emj.2005.034322.
- “Emergency Treatment for Suspected Opioid Overdose.” Chapter 381 Section 887 – 2021 Florida Statutes, State of Florida 2021 Legislative Statutes , 1 Jan. 2021.
- Cherrier, N., Kearon, J., Tetreault, R., Garasia, S., Guindon, E., “Community Distribution of Naloxone: A Systematic Review of Economic Evaluations.” PharmacoEconomics, ePublication, 11 November, 2021.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Washington, DC, American Psychiatric Association, (2013), p 541.
This article is part of the following sections: