Poison Control: Every Vape You Take…
E-cigarette, or vaping, product use associated lung injury (EVALI) is one of the hottest topics in emergency medicine. The Centers for Disease Control (CDC) is describing it as an “outbreak” due to rapid growth in cases over the last year. [1] As of November 13, 2019, there have been 2,172 cases of EVALI reported to CDC from 49 states and 42 confirmed deaths. [1] With new cases being reported daily, it’s important that providers become familiar with the information available in order to better assess potential cases.
Electronic cigarettes are portable devices that heat a liquid in order to aerosolize it for inhalation. These liquids most often contain nicotine, but may include a variety of other chemicals, including tetrahydrocannabinol (THC) or cannabidiol (CBD). [2] The main ingredient is usually solubilized in a hydrophilic vehicle such as propylene glycol or vegetable glycerin. The belief among many users of these devices is that fewer ingredients makes vaping a safer alternative to cigarettes. Because vaping is still relatively new, there is limited information available regarding complications associated with chronic use. However, at least six different groups of potentially toxic compounds have been identified in e-cigarette fluids, including nicotine, carbonyls, volatile organic compounds (benzene, toluene), trace metal elements, bacterial endotoxins and fungal glucans. No specific cause has been identified, but a reported 86% of 867 EVALI patients utilized THC-containing products, which makes their use a cause for concern.1 A common additive in these THC products is vitamin E acetate, which was recently found to be a potential chemical of concern in EVALI cases. In fact, CDC laboratory testing of bronchoalveolar lavage fluid samples from 29 patients found vitamin E acetate in all of the samples. [1]
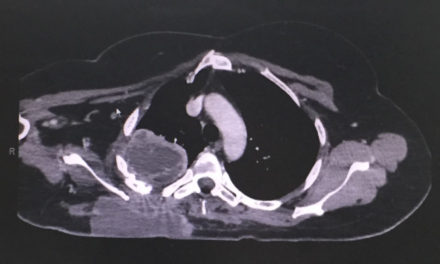
EVALI is considered a diagnosis of exclusion because no specific test exists to confirm its presence. A variety of symptoms are associated with EVALI. Respiratory symptoms are the most common, including cough, chest pain and shortness of breath. [3,4] Gastrointestinal symptoms are also prevalent, including abdominal pain, nausea, vomiting and diarrhea. In addition, constitutional symptoms including fever, chills and weight loss are frequently reported. Laboratory abnormalities in these patients may include elevated white blood cell count, serum inflammatory markers (C-reactive protein and erythrocyte sedimentation rate), and liver transaminases. Patients often have pulmonary infiltrates on chest x-ray and opacities on chest CT. Due to the nonspecific nature of these findings, healthcare providers should consider the possibility of other or multiple etiologies in their assessment.
At this time there are no specific guidelines on the management of EVALI, but the Department of Health and Human Services and the CDC have put together interim guidance for the treatment of the condition. [3] Corticosteroids may be considered, except in patients with suspected fungal infections, due to their effect on inhibition of the inflammatory response. 82% of 140 cases reported nationally to CDC improved on corticosteroids. There is no single dose suggestion for the use of steroids, so consultation with a pulmonologist may be considered. Patients who present with symptoms consistent with community-acquired pneumonia should be treated in accordance with the current guidelines. Patients should also be provided with education regarding the risks associated with vaping, with discontinuation advised. If successfully treated, patients should receive a follow-up evaluation within 1-2 weeks post discharge with consideration for additional follow-up at 1-2 months after discharge.
While there is no single known cause identified for EVALI, the one commonality among all cases is the reported use of e-cigarettes or vaping. In order to better characterize and treat this illness, CDC is stressing the importance of reporting cases to state, local, territorial or tribal health departments. [4] CDC is also accepting vaping-related products and devices, as well as laboratory specimens, for testing. Statistics and recommendations are updated and released on the CDC website regularly. [1]
With continued efforts from providers and health systems across the nation, the knowledge and treatment paradigms for this new threat continue to evolve and progress toward control of this outbreak. ■
FPICN toxicologists are available 24 hours a day, free of charge, at 1-800-222-1222 to answer any questions practitioners may have about EVALI or any other toxic exposure.
References
- CDC. Outbreak of lung injury associated with e-cigarette use, or vaping. Atlanta, GA: US Department of Health and Human Services, CDC; 2019. www.cdc.gov/lunginjury
- Christiani DC. Vaping-Induced Lung Injury. N Engl J Med. Sept 6. 2019.
- Siegel DA, Jatlaoui TC, Koumans EH, et al. Update: Interim Guidance for Health Care Providers Evaluating and Caring for Patients with Suspected E-cigarette, or Vaping, Product Use Associated Lung Injury — United States, October 2019. MMWR Morb Mortal Wkly Rep 2019;68:919–927.
- Layden JE, Ghinai I, Pray I, et al. Pulmonary Illness Related to E-Cigarette Use in Illinois and Wisconsin – Preliminary Report. N Engl J Med. Sept 6. 2019.
This article is part of the following sections: