Case Report: A Case of the Blues
HPI:
A 17-year-old female with PMH of juvenile dermatomyositis, duplicated IVC and oral contraceptive use, presented with a one-day history of left leg swelling, discoloration and pain. Earlier this month, she received intravenous immunoglobulin for her juvenile dermatomyositis. She denied any shortness of breath or history of thromboembolism.
T: 98.6, BP 137/87, Pulse: 129, Resp 18, 98% on RA
No respiratory distress. Left thigh was visibly swollen and discolored. Patient had monophasic L Dorsalis Pedis signals with Doppler. Patient had 5/5 strength with flexion and extension of the left hip and knee, and 5/5 strength with plantar and dorsiflexion of the ankle.
Labs:
D dimer 3.5 (Normal <0.5). Lupus anticoagulant, Anticardiolipin IgG, Beta 2 glycoprotein IgG, Protein C, Protein S, Antithrombin III activity, Factor V Leiden, Prothrombin Gene Mutation were all within normal limits. Pregnancy test was negative.
Imaging:
Venous Duplex Bilateral Ultrasound revealed a very large clot burden in the left lower extremity with a possible completely thrombosed common iliac vein. There was incomplete compressibility from the left common femoral vein to the left popliteal vein. Right lower extremity was unremarkable.

Fig. 1: Left Leg discoloration and swelling.
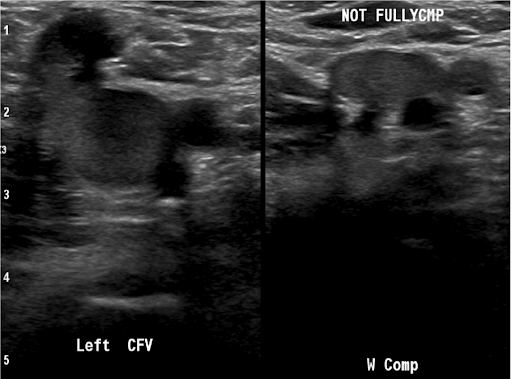
Fig. 2: Venous Duplex Ultrasound showing large clot burden in the left common femoral vein.
Management:
The patient was started on Eliquis after rheumatology and hematology consults. The patient was offered hospital admission, but she and her mother elected to undergo a trial of outpatient management. She was advised to stop oral contraceptive use. She returned one day later with increased swelling and pain. She was admitted to the hospital and underwent mechanical thrombectomy three days later, which showed extensive DVT throughout her left IVC, left renal vein, left iliac vein and left common femoral vein. She tolerated the procedure well and was discharged on Eliquis. Her follow up ultrasound three months later showed resolution of her DVT.
Discussion:
Phlegmasia cerulea dolens is a rare disorder in the spectrum of venous thromboembolism. Large clot burden in the venous system causes significant venous congestion and increased venous pressure leading to edema from increased extravasation of fluid into the subcutaneous tissue.
Thrombotic events are a known complication of immunoglobulin treatment. Proposed mechanisms include increased blood viscosity, activation of procoagulant factors, and vasospasm. Risk factors for thrombosis include a large first-time dose, OCP use, advanced age, hypercoagulable states, coronary artery disease, and ITP. The presence of four or more risk factors appears to be significantly associated with thrombotic events.
Juvenile dermatomyositis is a pro-inflammatory condition that increases risk of thrombotic events by creating a hypercoagulable state. The patient had additional multiple risk factors for a thrombotic event that included duplicated IVC, recent IVIG infusion, recent hospitalization, and OCP use. Proposed strategies to reduce the incidence of IVIG associated thrombotic events include reducing first administration dosing and slowing down infusion rates. ■
References:
- Daniel GW, Menis M, Sridhar G, Scott D, Wallace AE, Ovanesov MV, Golding B, Anderson SA, Epstein J, Martin D, Ball R, Izurieta HS. Immune globulins and thrombotic adverse events as recorded in a large administrative database in 2008 through 2010. Transfusion. 2012 Oct;52(10):2113-21. doi: 10.1111/j.1537-2995.2012.03589.x. Epub 2012 Mar 12. PMID: 22448967.
- Lee YH, Song GG. Idiopathic inflammatory myopathy and the risk of venous thromboembolism: a meta-analysis. Rheumatol Int. 2017 Jul;37(7):1165-1173. doi: 10.1007/s00296-017-3735-0. Epub 2017 May 10. PMID: 28493173.
- Lidar M, Masarwa S, Rotman P, Carmi O, Rabinowicz N, Levy Y. Intravenous immunoglobulins for rheumatic disorders and thromboembolic events-a case series and review of the literature. Immunol Res. 2018 Dec;66(6):668-674. doi: 10.1007/s12026-018-9047-y. PMID: 30565202.
This article is part of the following sections: