Ultrasound Zoom: POCUS For Shoulder Dislocation: Another Weapon in Your Clinical Arsenal
Introduction
I have always been an “in the trenches” kind of person. While the acuity, adrenaline rush, and hands-on aspects of emergency medicine certainly hold their appeal, I love this field because it so beautifully straddles both the most dramatic and the most humbling aspects of the medical profession. Emergency medicine is messy, both literally and figuratively. We see everything, and we see it before anyone else in the hospital. We often meet patients when they are in their most vulnerable states, and we wade daily through a sea of trauma, injustice, poverty, substance use, homelessness, mental health disorders, and other complex medical and societal issues. We are constantly investigating, teaching, advocating, stabilizing and treating—all while seeking the best and most efficient disposition for our patients. However, life “on the front lines” of the healthcare system can also be physically, mentally, emotionally and even spiritually grueling, especially given the unique time constraints under which we work. Successful physicians navigate these challenges by charging toward the battlefield, armed with every weapon at their disposal. Point-of-care ultrasound, or POCUS, is one of the most versatile and advantageous tools in the emergency medicine armamentarium.
Shoulder Dislocations: The Clinical Problem
I have heard some seasoned attending physicians remark that they have grown increasingly weary of the procedural aspects of emergency medicine over the course of their careers. They view procedures, such as shoulder reductions, as time and resource-heavy endeavors that add to the existing burden of life “in the trenches.” From a purely clinical perspective, shoulder dislocations are quite straightforward; they usually present with an obvious shoulder deformity, and they are treated with joint reduction techniques. However, in practice, the diagnosis and treatment of shoulder dislocations can be tedious and can send the emergency room workflow to a screeching halt.
When a patient’s presentation is suspicious for a shoulder dislocation, one generally begins by obtaining x-rays to confirm the diagnosis and rule out concomitant fractures. After each reduction attempt, one must then obtain more films to determine whether the procedure was successful. In my bustling and often chaotic urban, public hospital, where my colleagues and I work with limited staff and resources, we often encounter delays in obtaining timely imaging—even for portable films. Delays in obtaining the initial diagnostic x-rays can worsen the patients’ muscle spasms, making any attempted reductions more difficult. Additionally, obtaining multiple x-rays for shoulder dislocations–especially if several reduction attempts are required—further consumes time, staff and medical supplies, and increases the costs associated with the emergency room visit. It also exposes patients to more radiation, which can be particularly problematic if they are pregnant, if they are children, or if they have other contraindications to irradiation. Furthermore, many shoulder reductions are performed under procedural sedation, which requires additional staff and supplies at the bedside before, during and after the procedure.
The POCUS Advantage
POCUS is a wonderful weapon for more efficiently managing shoulder dislocations, even during the most tumultuous of shifts. POCUS spares the patient from radiation and provides real-time information about the success of a procedure at the bedside.
Shoulder POCUS or Traditional Radiograph?
How does shoulder POCUS compare with traditional radiographs, in terms of diagnostic accuracy? Can shoulder POCUS completely replace x-rays in the diagnosis and management of shoulder dislocations, or will it miss clinically relevant, concomitant fractures, which are known to occur in about a quarter of all shoulder dislocations?
Only a few small, prospective, observational studies have compared the diagnostic accuracy of POCUS and x-rays in the setting of shoulder dislocations & reductions. Although the sensitivities and specificities for diagnosing dislocations with POCUS ranged from the high 80s to 100% in nearly all the studies, the data cannot be generalized, due to both the heterogeneity of the study designs, and the level of ultrasound training among clinicians participating in the studies (ranging from POCUS-trained physicians to college students, who had completed a shoulder POCUS crash course). However, other studies have shown that the three main risk factors for concomitant fractures include older age, first time dislocating the joint, and a traumatic mechanism. If all three risk factors are absent, the negative predictive value for associated fractures is nearly 97%. Taking all of this into account, we cannot yet eliminate shoulder x-rays altogether, although some physicians might consider skipping a pre-reduction radiograph in favor of shoulder POCUS in a patient without major risk factors for concomitant fractures. However, POCUS is an excellent alternative to radiographs in determining the success of a reduction at the bedside, especially if multiple attempts are required, as this will save time, resources, and additional radiation. In other words, shoulder POCUS is more of a high-powered firearm than a military tank; it does not completely take us out of the clinical trenches, but it can help us fight our battles more efficiently.
Anatomy
Shoulder POCUS is quick and easy—even for a novice sonographer! It simply requires a functional ultrasound machine and a sound understanding of the anatomy of the glenohumeral joint. Frank Netter’s illustration (Figure 1) depicts the muscles and bony structures surrounding and overlying the glenohumeral joint in the posterior view. You will notice that the deltoid normally covers the supraspinatus, as well as parts of the other rotator cuff muscles that all attach laterally to the humeral head. The scapular spine is the bony demarcation of the supraspinatus and infraspinatus (located superiorly and inferiorly, with respect to the scapular spine), and it extends to the acromion posteriorly and the coracoid process anteriorly. A sound knowledge of these anatomic landmarks allows for seamless scanning.
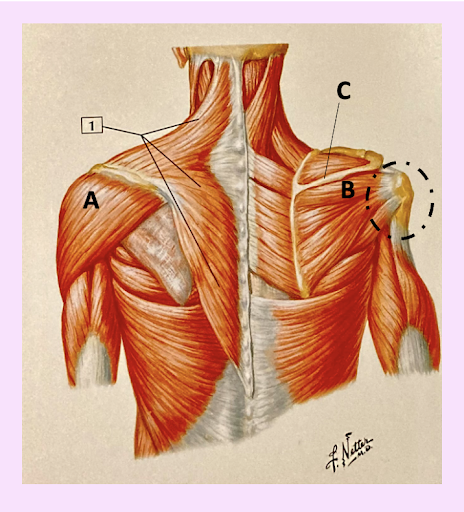
Fig 1: Posterior Shoulder muscles, as demonstrated in Netters’ Anatomy–cited accordingly, with additional labels, as follows: A) Deltoid. B) Infraspinatus. C) Scapular Spine. The dashed ellipse indicates the posterior view of the glenohumeral joint.
POCUS of the Normal Shoulder
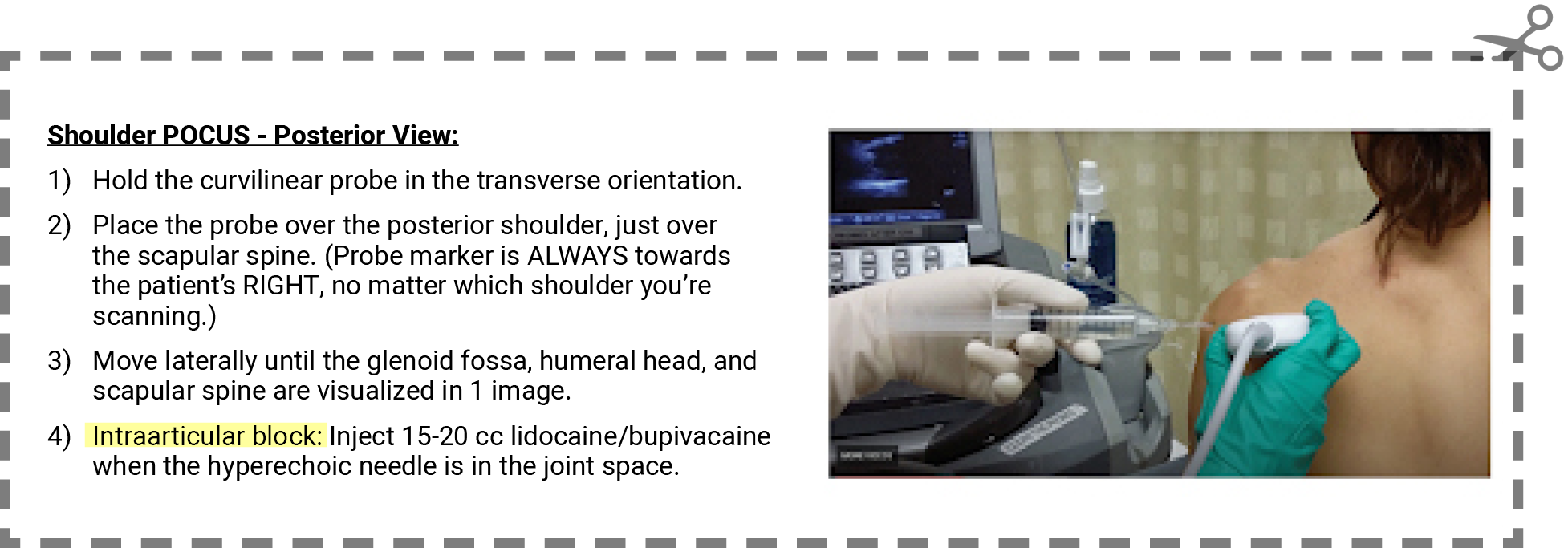
There are both anterior and posterior approaches to examining the shoulder with POCUS, but I have found the posterior approach to be the easiest to perform. Additionally, in several studies, the posterior approach has had slightly better sensitivities and specificities, when compared to the anterior approach. To perform shoulder POCUS via the posterior technique, it is best to use a curvilinear probe, although a linear probe may suffice, if the patient’s body habitus allows. Hold the probe in the transverse position, just over the scapular spine, with your probe marker directed to the patient’s right side (Figure 2). Move laterally until you see both the glenoid and the humeral head. Remember that all bony structures will appear hyperechoic, or white. Muscular structures will be more echogenic (i.e., somewhere in between grey and black), and any fluid will appear anechoic, or completely black.
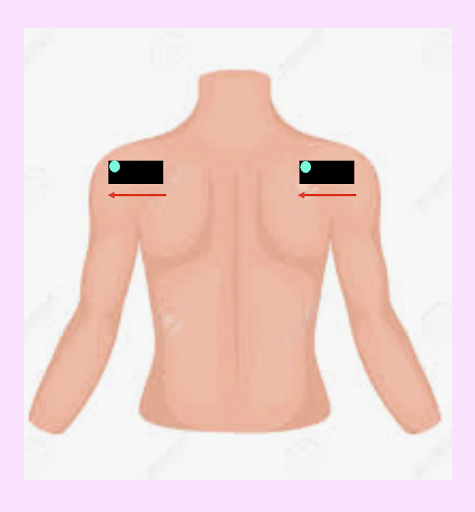
Fig 2: In this schematic for ultrasound probe orientation in the posterior shoulder POCUS view, the black box represents the curvilinear probe in the transverse orientation. The blue circle represents the marker/indicator on the ultrasound probe. The arrows are reminders to hold the probe in the transverse orientation, with the probe marker to the right, regardless of the shoulder you are examining; this is ultrasound convention.
In the posterior approach, the patient’s back (posterior) will be in the near field and the patient’s front (anterior) will be in the far field. As demonstrated in Figure 3, the scapular spine will be more medial, and the attachments of the rotator cuff muscles on the humeral head will be more lateral. Fanning the probe caudally, you will first see the deltoid muscle, followed by the infraspinatus as it attaches to the humeral head. You will then see the humeral head and the glenoid fossa. You may also see the hyperechoic scapular spine in the medial aspect of your image.
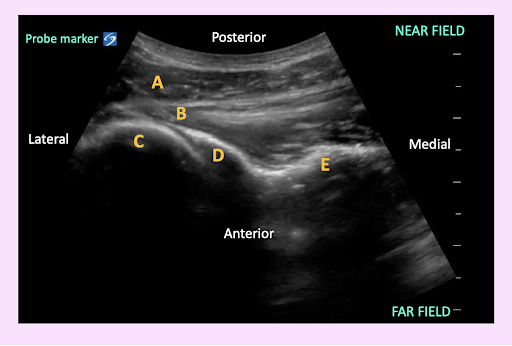
Fig. 3: In this view of a normal shoulder, one can identify the following structures in their proper anatomic locations: A) Deltoid, B) Infraspinatus attaching to the Humeral Head, C) Humeral Head, D) Glenoid Fossa, & E) Scapular Spine.
POCUS of Anterior & Posterior Shoulder Dislocations
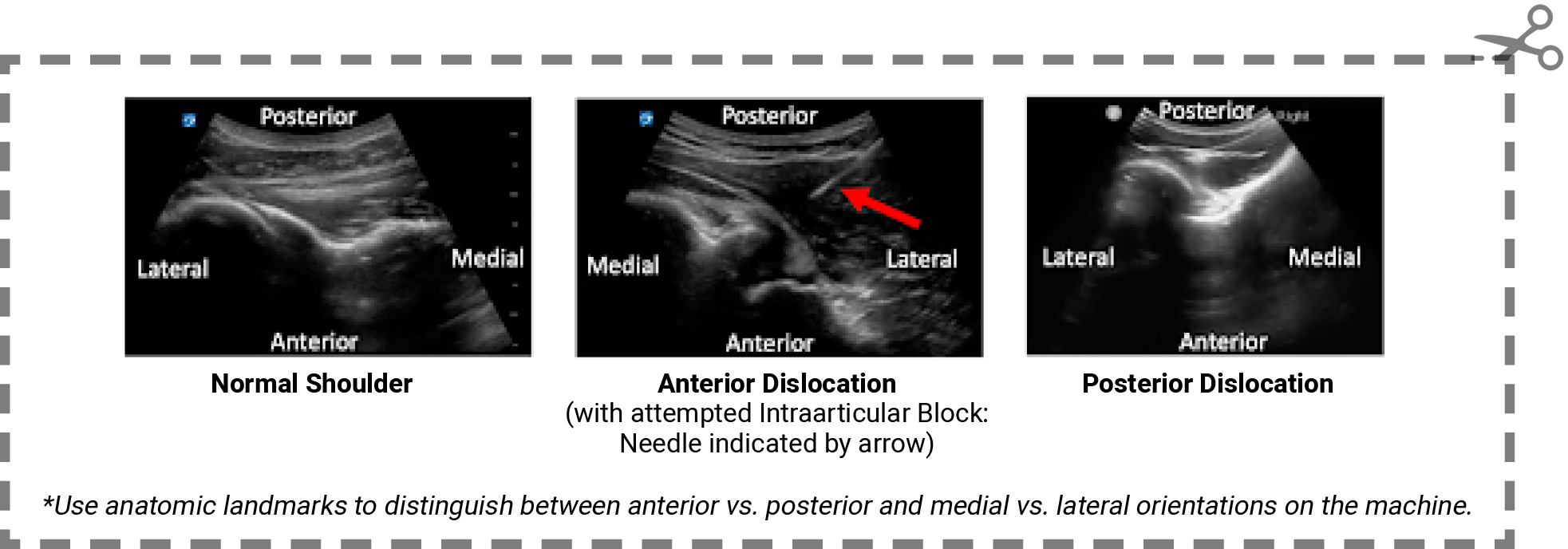
How does one identify shoulder dislocations, using the posterior POCUS approach? In an anterior dislocation (Figure 4), the humerus will be visualized closer to the far field, as it will be displaced more anteriorly, or further from the ultrasound probe. Therefore, the humeral head will appear to be below the scapular spine. A posterior dislocation (Figure 5) will show opposite image—the humeral head will be closer to the near field, as it will be displaced more posteriorly, or closer to the ultrasound probe. Therefore, the humeral head will appear to be above the scapular spine. Some studies have attempted to quantify the exact degree of anterior and posterior displacement on POCUS views, but these data are limited and not yet generalizable; at this time, it is probably best to compare your pre-reduction POCUS image with your post-reduction POCUS image to determine if your reduction attempt was successful. Note that the ability to visualize external rotation of the shoulder joint on the ultrasound also indicates that your reduction was successful. I recommend watching a video by Dennis D’Urso, MD, a former chief resident of my residency program, which demonstrates external glenohumeral joint rotation after a shoulder reduction (Video 1).
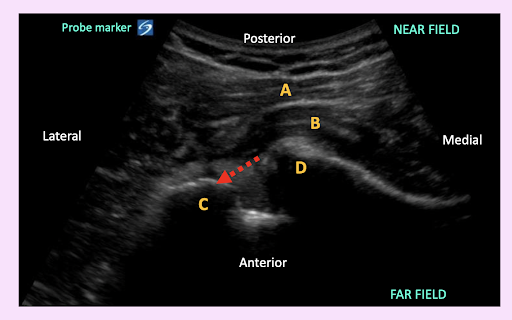
Fig. 4: An anterior dislocation is visualized when the humeral head appears to be below the scapular spine & glenoid fossa (i.e., more anterior, or closer to the far field), as indicated by the dashed arrow. Note the abnormal space in the joint, indicating the lack of articulation between the humeral head and the glenoid fossa. A) Deltoid. B) Infraspinatus. C) Humeral Head. D) Glenoid Fossa.
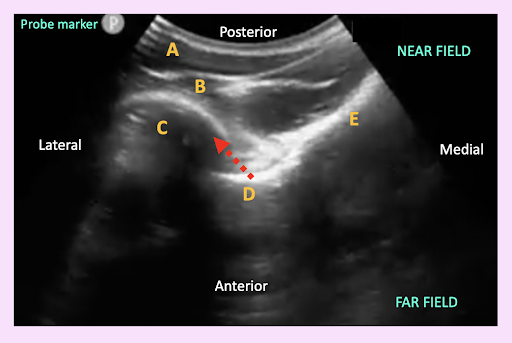
Fig. 5: A posterior dislocation is visualized when the humeral head appears to be above the scapular spine/glenoid fossa (i.e., more posterior, or closer to the near field), as indicated by the dashed arrow. Note the abnormal space in the joint, indicating the lack of articulation between the humeral head and the glenoid fossa. A) Deltoid. B) Infraspinatus. C) Humeral Head. D) Glenoid Fossa. E) Scapular Spine.
Video 1: Ultrasound Guided Intra-articular Block for Anterior Shoulder Dislocation. Dennis D’Urso, MD, courtesy of the UM/Jackson Health System EM residency ultrasound database.
POCUS for Pain Control: Intraarticular Block
Pain control also plays a major role in the success of a reduction procedure. While procedural sedation with intravenous medications is commonly used for shoulder reductions, several studies have explored the role of ultrasound-guided intraarticular blocks as alternatives to the time-consuming, costly, and often more complication-ridden procedural sedation techniques. The data are sparse: limited to a few, small randomized controlled trials that were heterogeneous in design, thus limiting their generalizability to emergency department care. Additionally, systematic reviews of these data have not shown any difference in the success rates of shoulder reductions with either technique. However, POCUS-guided blocks have been shown to significantly reduce the time, cost and complications associated with the procedure. Therefore, one should consider a POCUS-guided shoulder block in the right patient and setting.
Using the posterior POCUS approach to the intraarticular glenohumeral block (Fig 6a & 6b), first sterilize the skin over the shoulder. Next, find the glenoid and humeral head, using the previously discussed posterior POCUS approach. Next, simply inject 15-20 cc of 1% lidocaine into the joint space, visualizing your hyperechoic needle tip and the “bubbles” of hypoechoic anesthetic fluid in real time on the machine. (You can also use 2% lidocaine or bupivacaine, depending on what is easily available in your ED.) After waiting about 10-20 minutes, you can attempt to reduce the joint without procedural sedation. Dr. D’Urso’s video also demonstrates an ultrasound-guided intraarticular block in real time (Video 1).

Fig. 6a: This is the setup for a POCUS-guided intraarticular block in the posterior view. The curvilinear probe is placed on the patient’s posterior shoulder, with the probe marker pointing toward the patient’s right side, as indicated by the arrow.
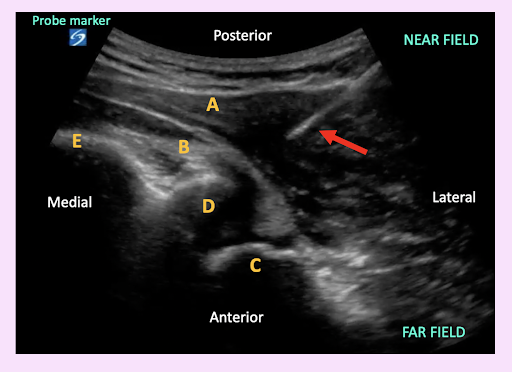
Fig. 6b: In this patient with an anterior shoulder dislocation, a lidocaine block was used prior to reduction. Visualizing the hyperechoic needle tip (indicated by the arrow) in the joint space and watching for “spreading” or “bubbling” of the anechoic lidocaine in this space ensures that the examiner anesthetizes the right area. A) Deltoid. B) Infraspinatus. C) Humeral Head. D) Glenoid Fossa. E) Scapular Spine.
Take-Home Points
The next time that you find yourself managing a patient with shoulder pain and an obvious upper extremity deformity while grappling with a particularly hectic shift, remember that shoulder POCUS is in your emergency medicine arsenal. Current evidence suggests that in most cases, you should still start by obtaining a plain radiograph to assess for concomitant fractures (unless your patient lacks the aforementioned risk factors). If fractures are not demonstrated on the initial x-ray, take up your gauntlet—I mean, probe—and capture a POCUS image of the patient’s dislocated shoulder. After employing your favorite reduction technique, reach for your probe again. Does the shoulder look reduced? If not, you can try again, as often as is necessary. You can track your progress in real time with the ultrasound, rather than pausing to hammer-page your radiology tech for additional scans, or to re-dose analgesics while waiting for the portable film. Additionally, in the right patient, a POCUS-guided intraarticular lidocaine block may provide pain control without the need for procedural sedation during reduction attempts. Using shoulder POCUS, your patient will likely be ready for disposition much sooner, and you will have saved time, energy and resources—all of which you can dedicate to the other battles that you valiantly continue to fight each day on “the front lines.” ■
Shoulder POCUS To-Go:
References:
Must-Read/Must-View Sources are in bold.
Bafuma, P. (2016, Mar 22). Clinical Question: How effective is intra-articular lidocaine for shoulder reduction? Canadiem.
D’Urso, D. Ultrasound-Guided Intraarticular Block for Anterior Shoulder Dislocation. [Video]. YouTube. Accessed August 2021.
Hansen, JT. Netter’s Anatomy Flash Cards: Companion Atlas of Human Anatomy 6th Edition. 4th Edition. Elsevier/Saunders, 2014.
Gottlieb, M, et al. Point-of-care ultrasound for the diagnosis of shoulder dislocation: A systematic review and meta-analysis. American Journal of Emergency Medicine 37: 757-761. 2019.
Gottlieb, M, and Russel, F. Diagnostic Accuracy of Ultrasound for Identifying Shoulder Dislocations and Reductions: A Systematic Review of the Literature. West JEM. 2017. DOI: 10.5811/westjem.2017.5.34432
Lahham, S, et al. Pilot Study to Determine Accuracy of Posterior Approach Ultrasound for Shoulder Dislocation by Novice Sonographers. West JEM. 2016. DOI: 10.5811/westjem.2016.2.29290.
Nagdev, A. Ultrasond-Guided Glenohumeral Joint Evaluation and Aspiration. (2016, June 15). ACEP Now.
Richardson, L. (2018, Aug 4). POCUS Triage Shoulder Dislocation. Emergency Medicine St. John.
Rich, C. (2016, Nov 30). POCUS: Shoulder Dislocation. Brown Emergency Medicine: Orthopedics, Procedures, Trauma, Ultrasound.
Riguzzi, C, Mantuani, D, and Nagdev, A. (2014, Feb 12). How to Use Point of Care Ultrasound to Identify Shoulder Dislocation. ACEP Now.
Seyedhosseini, J, et al. Accuracy of point-of-care ultrasound using low frequency curvilinear transducer in the diagnosis of shoulder dislocation and confirmation of appropriate reduction. Turkish Journal of Emergency Medicine 17:132-135. 2017 .
Sherman, SC, et al. (2020). Shoulder dislocation and reduction. UpToDate. Retrieved 15 March, 2021.
Tin, J. (2018, Jan 8). US Probe: Ultrasound for Shoulder Dislocation and Reduction. emDOCS.
This article is part of the following sections: