Bleeding from a Chronic Head Wound
The patient had fallen the day before, and it was uncertain as to why the wound was bleeding today, or if it had been bleeding intermittently since his fall. The patient was a poor historian; he was unable to tell us how long he had had the wound, what the reason for the wound was, or what treatment had been offered or accepted. He just stated that, “they wanted to do surgery that would have taken a skin flap from my forehead and grafted it onto my scalp. They said I would lose my eyebrows, and I didn’t want that.” Throughout the visit he alternately said the wound and the consultation had been “just a few months ago,” to “a few years ago,” to “a while ago.” No family was present to give more information.
 The patient was admitted, the area biopsied, and diagnosed as cutaneous squamous-cell carcinoma with invasion of the calvarium. Because of the locally advanced progression, he was not a candidate for surgery or radiation treatment.
The patient was admitted, the area biopsied, and diagnosed as cutaneous squamous-cell carcinoma with invasion of the calvarium. Because of the locally advanced progression, he was not a candidate for surgery or radiation treatment.
Cutaneous squamous-cell carcinoma is the second most common skin cancer [1]; only basal-cell carcinoma has a higher incidence. There are 5.4 million basal cell and squamous cell carcinomas diagnosed each year, of which approximately 80% are basal cell carcinoma. The incidence of squamous cell carcinoma in Caucasians is 0.1-0.15% per year, and peaks in the mid-60s. Risk factors include chronic sun exposure, male sex, Caucasian, advanced age, fair skin that is sensitive to ultraviolet radiation (blonde or redhead), blistering sunburns, a history of actinic keratosis (a premalignant condition), HIV, tobacco use, and immunosuppression, including those being treated for solid organ tumors. In 2012, an estimated 3900 to 8700 people in the U.S. died from cutaneous squamous cell carcinoma.
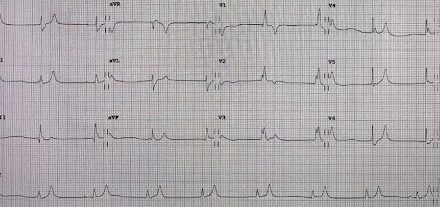
Surgery is the first line of treatment for skin cancer. In more than 95% of patients, the cancer is cured with surgery. Concerns about the effect on appearance are one of the most important issues to patients, such as this one. In a small percentage of patients, the tumor reaches an incurable state because it becomes metastatic or has locally advanced progression and is no longer amenable to surgery or radiation therapy. For patients with locally advanced or metastatic cutaneous squamous-cell carcinoma, the immune checkpoint inhibitor cemiplimab can induce a response in approximately half the patients. Palliative systemic therapy was offered and declined by the patient. Additionally, our patient was found to have a new diagnosis of a blood dyscrasia.
In summary, the patient presented with bleeding from a chronic head wound, was found to have both squamous-cell carcinoma and a new blood dyscrasia. While there is the potential for treatment of one of both of these cancers, the patient chose to forego potential curative and/or palliative treatment and was discharged home with hospice per his expressed wishes. ■
References:
- K.S. Nehal and C.K.Bichakjian. “Update on Keratinocyte Carcinomas.” NEJM. Vol 379 No 4 p. 363.
- “Key Statistics for Basal and Squamous Cell Skin Cancers.” The American Cancer Society. Jan. 8, 2020. Access at www.cancer.org/cancer/basal-and-squamous-cell-skin-cancer/about/key-statistics.html
- M.R. Migden et al. “PD-1 Blockade with Cemiplimab in Advanced Cutaneous Squamous-Cell Carcinoma.” NEJM Vol 379 No. 4 p. 341
This article is part of the following sections:
Samantha manages fcep.org and publishes all content. Some articles may not be written by her. If you have questions about authorship or find an error, please email her directly.