Case Report: Extensive Pneumomediastinum in a 20-Year-Old
A 20-year-old female presented “emergently” from an Urgent Care complaining of nausea, vomiting, diarrhea and facial swelling with crepitus. She presented to a Midwestern Community Hospital with an EM residency associated with a large academic university, and with several tertiary referral centers in a 60-90 mile radius.
She had intractable nausea, vomiting and diarrhea since waking, and several hours later she felt and heard a “pop.” Shortly thereafter, her boyfriend noticed some right sided facial swelling. It is now on her bilateral face, and has spread to her neck and proximal/mid chest over the past few hours.
She complains of a burning raw feeling of pain from her stomach to her esophagus, and to her throat. She has a sensation of fullness, and it hurts to take a deep breath and to swallow, but not to talk or breathe. She denies fever, chills, dizziness, dehydration or other systemic signs or symptoms beyond what was noted above. Her mom notes that her voice sounded like it did before she needed a tonsillectomy and adenoidectomy.
Physical Exam
General: She appears moderately anxious and in mild distress, otherwise healthy, non-toxic, and well appearing.
Skin: Warm, dry, normal color, no rash, with palpable crepitus in the neck and anterior chest; can visualize fullness/swelling in the face but no skin irregularities on the face or torso.
Eyes: Pupils equally round, extraocular movements intact, clear conjunctiva, normal sclera.
HEENT: Normocephalic atraumatic, moist mucous membranes, bilateral moderate cheek fullness.
Neck: Mildly tender to palpation, supple without nuchal rigidity, mild fullness, full range of motion.
Pulmonary: Clear to auscultation without wheezes, rhonchi or rales, no accessory muscle use, no stridor, normal excursion.
Cardiovascular: Regular rate and rhythm with normal heart sounds and without murmurs.
Gastrointestinal: Soft, non-tender, non-distended, normal bowel sounds, no crepitus.
Lymphatics: No edema in lower extremities.
Musculoskeletal: Extremities are non-tender and have no gross deformity, redness or swelling.
Neurologic: Alert and oriented x 3, GCS 15, normal mentation and speech, stable gait (as seen ambulating to the bathroom).
Psychiatric: Normal except as noted previously, clear and linear thought process.
Differential diagnosis: Pneumomediastinum consistent with Mallory Weiss tear; rule out Boerhaeve’s, will empirically treat with antibiotics, get Xrays (XR), CT’s, IV fluid rehydration, control nausea, consult as needed.
Imaging results
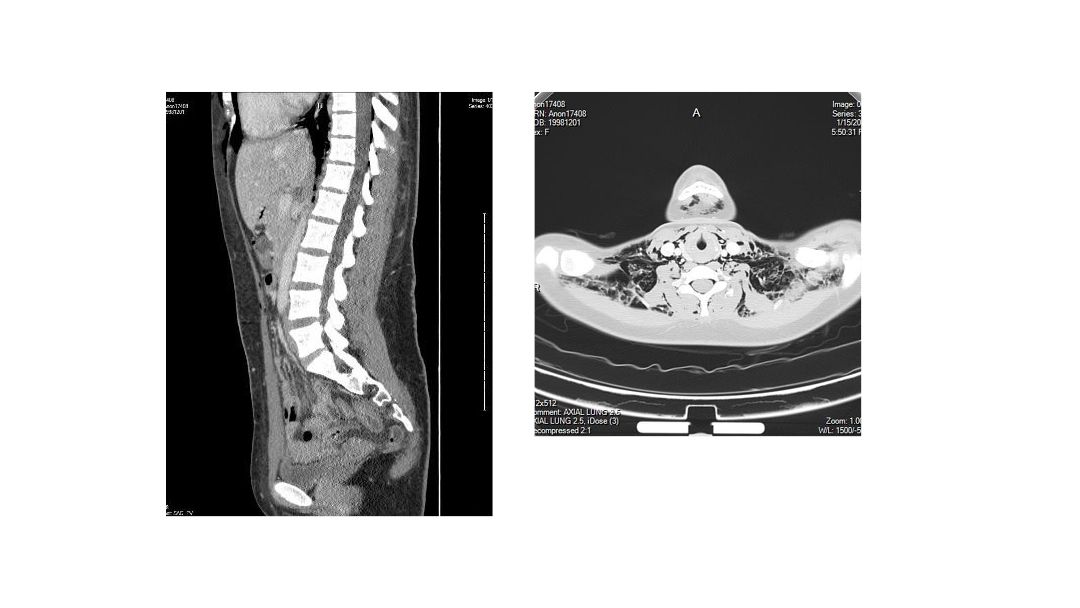
Chest XR: Extensive SQ air bilaterally into neck and into the abdomen, as well as pneumomediastinum. No definite pneumothorax, heart normal.
Soft Tissue neck XR: Extensive subcutaneous (SQ) air extending into the chest/mediastinum and up into the scalp.
CT chest/abdomen/pelvis with contrast: Extensive SQ air bilaterally that anteriorly extends to overlie the pelvis just superior to the pubic symphysis. Abnormal air extends down the thorax within the mediastinum and probably into the pericardial space. It also extends down the abdomen within the retroperitoneum and along the fascial planes. Questionable very small amount of free intraperitoneal air. Abnormal air also extends within the thoracic spinal canal from T1 to T11. Etiology for the extensive abnormal air collections are not clear from the CT. No obvious hole in the trachea or esophagus was seen.
Emergency Department (ED) course: Radiologist called the ED regarding the above results, and recommended further discussion with both cardiothoracic surgery and neurosurgery given the concerns about air in the pericardium and air in the spinal canal. “This is the most extensive pneumomediastinum I’ve seen in nearly 40 years of radiology.”
Cardiothoracic surgery recommended gastrograffin study to look for communication between the esophagus to the mediastinum, and agreed with transfer to a tertiary care center, as “95% of what I do is cardiac bypass surgery, and no other major chest surgery.” He also had not seen this extensive of a pneumomediastinum before.
Neurosurgery reviewed the films, disagreed about air in the spinal canal, asked about connective tissue disease history, recommended a head CT to rule out air in the brain, and also recommended transfer to the tertiary care center.
Discussion
Pneumomediastinum is an uncommon entity.
Pneumomediastinum can occur after surgery, infection, forceful coughing, vomiting, sneezing or VALI (Vaping Associated Lung Injury) due to the increased intrathoracic pressure causing air to enter the mediastinum from the lungs or airways. It can also be caused by barotrauma (scuba diving), as a result of childbirth, or cocaine and other drug abuse. [1-4]
Pneumomediastinum can be asymptomatic or can cause mild to moderate chest pain, voice change, cough, or stridor, as seen in this patient. Pneumomediastinum alone does not require further testing or intervention, unless the patient is symptomatic. In that case, a search for other injuries (larynx, trachea, pharynx, esophagus) is warranted.
Traditionally pneumomediastinum is limited to the mediastinum, and is treated with observation and reassurance, as the body will gradually reabsorb the air. What made this case unique was the extent of the subcutaneous air; circumferentially including both anterior and posterior planes from the pubic symphysis to the scalp; more extensively than any of the four specialists (emergency medicine, radiology, neurosurgery, and cardiothoracic surgery) had ever encountered prior.
Disposition: The patient was discharged home from the tertiary care institution the following afternoon after a period of observation; no intervention was needed. ■
References:
- https://medlineplus.gov/ency/article/000084.htm
- Tintinalli’s Emergency Medicine a Comprehensive Study Guide 9e, chapter 261, Pulmonary Trauma
- N Engl J Med 2018; 378:el
- J. Layden, M.D. et al, “Pulmonary Illness Related to E-Cigarette Use in Illinois and Wisconsin-Final Report,” N Engl J Med 2020; 382:903-916
This article is part of the following sections:
Samantha manages fcep.org and publishes all content. Some articles may not be written by her. If you have questions about authorship or find an error, please email her directly.