Ultrasound Zoom: Lung Ultrasound in the COVID-19 Pandemic
Have you ever asked yourself how your ultrasound probe can be used to fight the COVID-19 pandemic? Well, read on.
In my experience, point-of-care lung ultrasound (POC-LUS) has been invaluable in the bedside assessment of patients with respiratory complaints, helping to differentiate among the most common diagnoses, including congestive heart failure, pneumonia, pneumothorax or COPD. Now, I can add COVID-19 to my list!
In the setting of a pandemic, rapid case identification and severity stratification are crucial. RT-PCR of a nasopharyngeal specimen is the current standard for diagnosis, with rapid testing turnaround time approaching 1 hour or less. Meanwhile, patient disposition is determined — and often delayed — by a combination of clinical and radiographic assessment.
Noncontrast chest CT is highly sensitive (approximately 97%) for detecting the usual lung changes seen in COVID-19; however, it has several limitations preventing its widespread use, including availability, cost, radiation exposure, requirement for the patient to leave the evaluation area, and necessary cleaning between patients. Portable chest X-ray is often more rapidly available; however, it has poor sensitivity (approximately 65%), limiting its reliability as a screening or stratifying tool.
POC-LUS has proven to be an excellent imaging modality for COVID-19. First, the disease tends to follow a peripheral to central progression, making it amenable to surface imaging even in its earliest stages. In fact, the sensitivity of POC-LUS for detecting COVID-19 pneumonia can approach or even exceed that of chest CT.
Furthermore, POCUS has utility beyond lung imaging alone. A more extensive evaluation of dyspnea can be performed in the same bedside assessment by evaluating the heart and IVC in addition to the lungs. This “triple scan” can provide important information such as left ventricular function, presence of right ventricular strain, and volume status to further guide patient care.
Additionally, POCUS is portable, inexpensive, rapid, and therefore easily repeatable, making it an effective tool for monitoring the progression of disease and recovery without exposure to ionizing radiation. POC-LUS has been successfully utilized to determine responsiveness to alveolar recruitment maneuvers such as proning and mechanical ventilation, as well as to guide mechanical ventilation weaning and extubation.
Technique
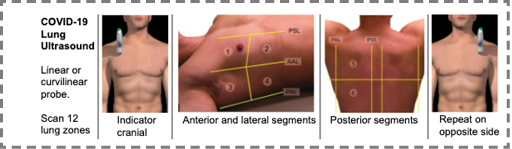
Probe: High-frequency linear or curvilinear probe
Settings: Select the lung preset (or manually disable filters and tissue harmonics; lung ultrasound is based on artifacts!). Use adequate depth to visualize the pleura and peripheral parenchyma, less than 5 cm to evaluate the pleural line, and more than 15 cm to evaluate B-lines.
Position: Seated positioning is preferred. Lateral decubitus positioning may be required to access all lung fields (e.g. in patients lying supine or prone).
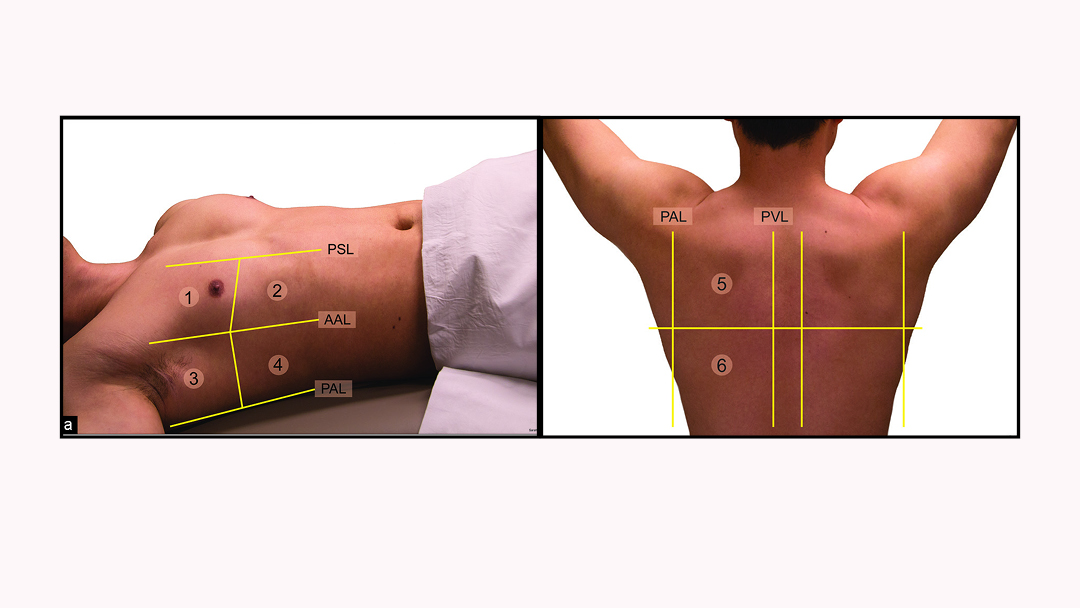
Technique: Orient the probe marker cephalad. Systematically scan the lungs in “lawn mower” fashion in 12 zones (upper and lower portions of the anterior, lateral, and posterior segments of each lung) as demonstrated in Figure 1.
Findings
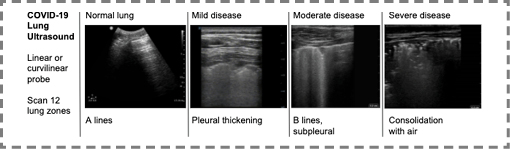
The typical CT pattern of COVID-19 is a diffuse bilateral interstitial pneumonia, with “ground glass” infiltrates primarily affecting the bases. Investigators in China and Italy have demonstrated that these infiltrates can be identified on ultrasound as B-lines; the density and scope of these B-lines were found to correspond with both CT findings and the clinical condition of the patients. Additional lung ultrasound findings are summarized in Figure 2 and include 1) a thickened pleural line, 2) multifocal B lines ranging from discrete to confluent, 3) small subpleural consolidations, and 4) large consolidations with air bronchograms. Small pleural effusions are sometimes present, however large effusions are suggestive of alternative pathologies. Figure 3 demonstrates ultrasonographic images of these changes.
While no imaging findings are specific for COVID-19, the constellation of these POCUS-LUS findings in the setting of a clinical picture with high pretest probability is strongly suggestive of COVID-19. Next time you evaluate a patient presenting with dyspnea, make sure to bring your ultrasound for a quick visual assessment that may support a rapid diagnosis and disposition!
Limitations
For those without any prior ultrasonography experience, a short training session in knobology will be useful; otherwise, the technique of lung scanning is simple and the interpretation is fairly straightforward.
A recognized limitation of lung ultrasonography is that it cannot detect lesions that are deep within the lung, as aerated lung blocks transmission of ultrasound waves. Chest CT is required to detect pneumonia that does not extend to the pleural surface.
Finally, adequate safety measures are required to prevent disease transmission. At minimum, the ultrasound probe and the machine in its entirety should be cleaned with an appropriate cleaning solution after each use. During this pandemic, additional measures such as covering the probe and machine in a protective barrier is recommended — especially during any aerosolizing procedures. ■
References
- Nazerian P, Volpicelli G, Vanni S, et al. Accuracy of lung ultrasound for the diagnosis of consolidations when compared to chest computed tomography. Am J Emerg Med. 2015;33(5):620–625
- Wu J, Wu X, Zeng W, et al. Chest CT findings in patients with coronavirus disease 2019 and its relationship with clinical features. Invest Radiol. 2020
- Peng Q, Wang X, Zhang L. Findings of lung ultrasonography of novel corona virus pneumonia during the 2019–2020 epidemic. Intensive Care Med. 2020
- Smith, et al. Point‐of‐care lung ultrasound in patients with COVID‐19 – a narrative review. Anaesthesia. 2020
- Is Superior to Plain Radiography in the Diagnosis of Pneumo-peritoneum.” British Journal of Surgery, vol. 89, no. 3, 2002, pp. 351–354., doi:10.1046/j.0007-1323.2001.02013.x.
- Grassi, Roberto, et al. “Gastro-Duodenal Perforations: Conventional Plain Film, US and CT Findings in 166 Consecutive Patients.”
- European Journal of Radiology, vol. 50, no. 1, 2004, pp. 30–36., doi:10.1016/j.ejrad.2003.11.012.
- Hefny, Ashraf, and Fikri Abu-Zidan. “Sonographic diagnosis of intraperitoneal free air.” Journal of Emergencies, Trauma, and Shock, vol. 4, no. 4, 2011, p. 511.
- Karahan, Okkes Ibrahim, et al. “New Method for the Detection of Intraperitoneal Free Air by Sonography: Scissors Maneuver.” Journal of Clinical Ultrasound, vol. 32, no. 8, 2004, pp. 381–385., doi:10.1002/jcu.20055.
- 1Asrani, Ashwin. “Sonographic Diagnosis of Pneumoperitoneum Using the ‘Enhancement of the Peritoneal Stripe Sign.’ A Prospective Study.” Emergency Radiology, vol. 14, no. 1, 2007, pp. 29–39., doi:10.1007/s10140-007-0583-3.
- Indiran, Venkatraman, et al. “Enhanced Peritoneal Stripe Sign.” Abdominal Radiology, vol. 43, no. 12, 2018, pp. 3518–3519., doi:10.1007/s00261-018-1628-7.
This article is part of the following sections: