Fall 2021: Daunting Diagnosis
Question:
A 63 year-old female presents to the emergency department with diffuse abdominal pain and “black discoloration” on her abdominal wall. The patient has a history of ovarian cancer, which was treated in 2014, opiate abuse, and known abdominal hernia. Patient presents febrile and hypotensive.
A photograph of her abdomen is below, along with a CT of her abdomen and pelvis. What clinical condition does the patient have?
Image 1: Abdominal wall with necrotic tissue

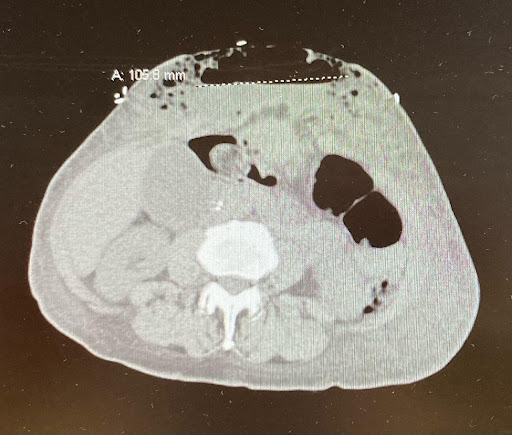
Image 2: Abdominal/Pelvis CT showing extensive fluid collection and development of air-fluid level with extensive amount of gas pockets and severe diffuse subcutaneous edema
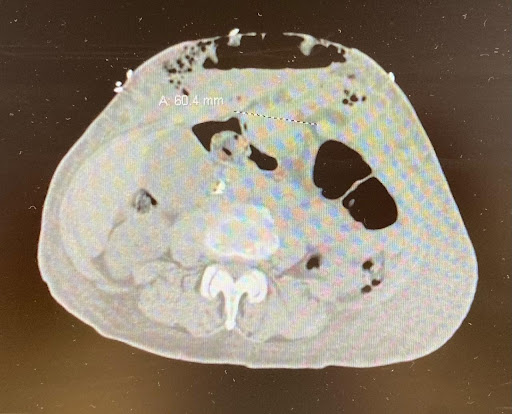
Image 3: Abdominal/Pelvis CT showing 6 cm ventral hernia with protrusion of omental fat
Answer:
The CT scan shows extensive inflammatory changes of the abdominal wall including an air-fluid level and subcutaneous gas concerning for superimposed infection with a gas-forming bacteria. The inflammatory changes are associated with a large, incarcerated ventral hernia and bowel perforation.
The patient was hemodynamically unstable, requiring sepsis protocol and emergent general surgery consultation.
The patient underwent an initial exploratory laparotomy for a necrotizing soft tissue infection, and multiple subsequent surgeries including resection of the transverse colon, multiple debridements of the anterior abdominal wall, open cholecystectomy, multiple wound wash-outs, and wound vac placement.
The patient additionally underwent hyperbaric treatment. Hematology was consulted for further treatment of her ovarian cancer. The patient’s prognosis is poor.
This article is part of the following sections: