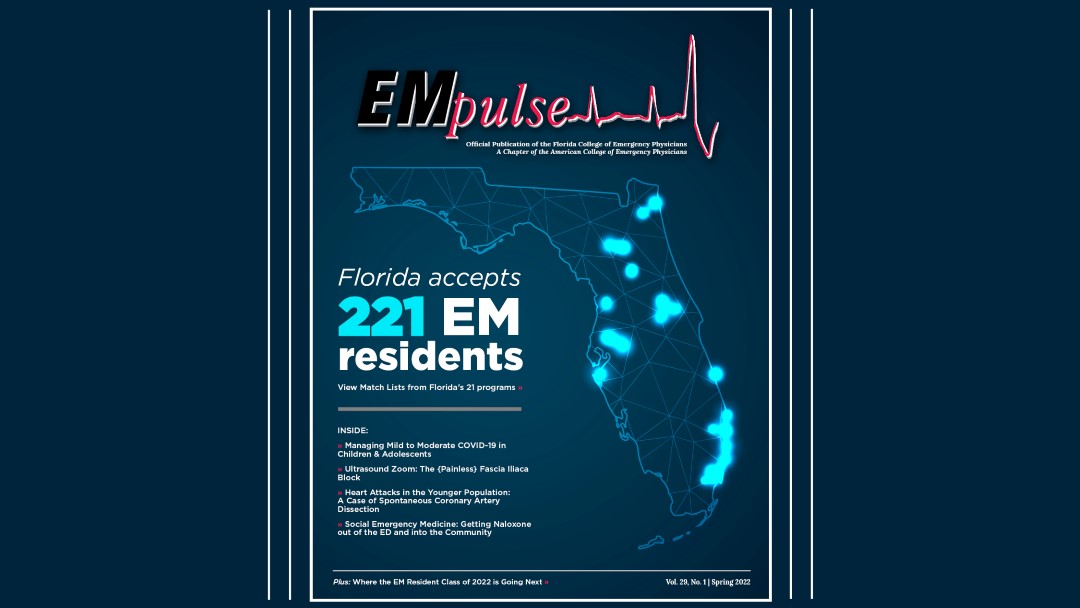
Spring 2022: Early Career Physicians
It’s 4:00 am in the ED. The end of your shift is in sight, and the empty room in the back corner is inviting you to take a nap. You might have even forgotten for a moment that the shift is single coverage, since the ED has gotten so quiet — I mean, chill. And then it happens: the patient who comes in with everything wrong, needing resources you don’t have. Appropriately caring for this patient requires medications that aren’t in your Pyxis, specialists that aren’t on call, and, oh, by the way, needing that procedure you’ve never done. You know the one I mean: the procedure you’ve secretly hoped for and dreaded, the one you had the lucky misfortune to avoid in residency. It’s the horrifying moment when you look around for an attending and realize, it’s YOU! So, you look for a smarter attending: an “attendier” attending.
Every physician in their early career has had this moment. If you haven’t yet, you will. Although you can’t entirely prepare for them, you can have a plan—and that, somehow, makes it just a little bit easier.
1. Reach for your resources.
Some physicians in their early career feel a mild sense of embarrassment when they use reference materials while on shift, especially when you’ve been out for a few years. Don’t feel embarrassed about this. Anyone with perfect recall of the full breadth of medical knowledge is either fictional or already being studied in Area 51. Our scope is enormous, and we chose a field that requires a lifetime of learning. It doesn’t make you a bad doctor if you need to look up how to place a chest tube because you haven’t done one in two years, or if you can’t remember all of the pediatric ACLS doses. If you feel self-conscious, you can say out loud, “I just want to double check to make sure I got this right.” Practicing emergency medicine is an open book test. Take the win.
2. Call a consult.
Yes, even at 4:00 am. When I use the term “consult” here, I don’t just mean specialists. Think about your former attendings, mentors, colleagues, or EM friend groups. Someone is bound to be up at any time of night. Consider your former residency classmates, who know exactly what you’re going through. At odd hours, talk to a fellow EM doc in another time zone, a nocturnist, or a medical social media group (while keeping HIPAA in mind). Talking through a clinical scenario can help give you new ideas, or catharsis after a tough case. Healthcare functions as a team system because we benefit from the input of multiple minds. Don’t forget about the knowledge of your RTs, veteran ER nurses, or other in-house staff who might have a solution to that major problem in your resuscitation, devastating equipment failure, or whatever weird circumstance arises. Recognize your limitations.
On the topic of actual specialist consultations—don’t be afraid to call a consult, even in the middle of the night. If you’re in a sticky situation that overlaps with the territory of another specialty, get them involved. The worst thing they can say is “sorry, I can’t help,” and the best thing they can say is something that will save your patient’s life.
3. Trust your gut.
You trained for this. Trust the years of residency training that were designed to prepare you for this moment. In those moments of paralyzing indecision, go back to the basics if you need to: the ABCs. You know how to improvise. Follow your instincts. Despite the multiple flaws in the world of medicine pictured in House of God, they did get one piece of advice right: “the first procedure is to take your own pulse.” Slow down and assess the situation. Focus on doing what you can.
In those terrifying moments that come, you won’t be able to save every patient. Some days we fight the god of death and lose. Even though it might feel like you’re alone, you aren’t. You’ve got resources. You’ve got colleagues. Most importantly, you’ve got a residency-trained emergency medicine physician: YOU. ■
This article is part of the following sections: