A Steadfast Approach to the COVID-19 Pandemic
Adaptability and agility: two words that describe one aspect of emergency medicine, and two qualities that we, along with all physician specialties, must continue to exercise on a daily basis in this COVID-19 pandemic.
Over a month ago, we were looking at an outbreak in China, Italy, South Korea, and Iran. Thirty days ago, the number of cases in the U.S., including those repatriated from the Diamond Princess cruise ship, was in the double digits. As of this writing, there are over 385,000 cases in the US [1,2]. A state of emergency has been declared, and “shelter-in-place” and social distancing are the norm. Powerhouse companies such as Hanes, Ford, and General Motors have converted to manufacturing ventilators and masks. Our country is adapting. On the front lines, we are also adapting. Daily, our inboxes and online meetings are full of new testing procedures, new PPE requirements, new emergency department patient flow diagrams, and new respiratory isolation policies and procedures. Our innate adaptability and agility, in the field of emergency medicine, are key components of our endurance and success in fighting this virus. We cannot forget: we are adaptable and agile human beings.
We have learned a great deal about the virus already. Before SARS-CoV-2 was even known, we had all heard frequently of novel viruses morphing via antigen shift and drift. Mutations allowing viruses to move from animal hosts to humans is not a new or novel concept. We all knew, from microbiology classes many years ago, that given probability and time, once in a great while a virus will succeed in shifting its RNA in such a way that the virus is “optimized” for human survival. This is one of those times.
The “ideal virus” would spread human-to-human readily, replicate quickly, and avoid making its host too sick before being exposed to many other human hosts (along with asymptomatic carriers that are difficult to identify). The ideal virus is not overly deadly, and it is easily transmissible. Strains of influenza such as H1N1 caused a pandemic in such a way. Similarly, the novel strain of coronavirus reached a pandemic phase just 2-3 months after the pathogen’s emergence. Healthcare professionals and researchers already have had great experience in dealing with viruses, including those that are easily transmissible as well as dangerous. The flu is a great example. But in these times, we have challenged our knowledge, pushed the boundaries on antiviral therapy, applied old knowledge to new situations, and have made great strides in determining how this virus is transmitted, how to treat it, and even the beginnings of a vaccine to mitigate its effects. We are grateful to the many researchers and clinicians who are sharing their knowledge and experience—from N95 reuse and sanitation, to drug combinations to combat the virus and safe intubation strategies. We as clinicians will remain adaptable. We will stay up hours after our tiresome shift to read more about the virus, gain new knowledge, and work with healthcare leadership to advocate for the best practices.
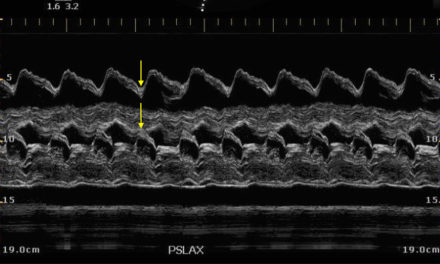
The virus first emerged in humans as early as December 2019 in Wuhan, China. It was a respiratory viral infection that, at first, perhaps did not seem terribly different from other upper and lower respiratory tract infections that are easily transmissible, especially in close quarters such as the seafood and live animal market where the virus first emerged. But healthcare workers noticed a pattern. This virus showed a unique, pneumonia-like airspace pattern on radiographic imaging, and on January 7, 2020, China identified the pathogen’s RNA as a novel coronavirus. SARS and MERS are of the same coronavirus family. As January progressed, we saw an epidemic striking: the Hubei Province and Mainland China were at the center of the attention, but cases among travelers had emerged across the globe [3]. Notably the cruise ship docked in Japan, held for quarantine just as it was planning for disembarkation, went from one case to over 500 cases within just two weeks [2]. Italy, South Korea, and Iran then began to fight their own internal outbreaks [3]. The virus is undoubtedly spreading through U.S. communities, and a state of emergency has been declared in Florida as of March 1, 2020 [4].
We are gaining knowledge and adapting our practices to match this knowledge: epidemiology, risk factors, early presenting symptoms, transmission, and treatment. Initially, the practice was that a positive flu or viral panel essentially meant SARS-CoV-2 was highly unlikely to be present. However, data out of California suggest a 23% co-infection rate with other viruses. This type of data changes testing and risk stratification vastly. In terms of presenting symptoms, we’ve learned that less than half of patients have fever on initial presentation, that gastrointestinal symptoms should not be disregarded, and that anosmia and dysgeusia may be symptoms in otherwise asymptomatic carriers [5]. We’ve narrowed down that the virus lives longer on plastic than cardboard, and are storing masks in paper bags instead, just in case this helps [6].
ACE2 is the cell’s entry receptor for SARS-CoV-2. In addition to this receptor being located in both the respiratory and GI tracts, leading to a variety of symptoms, ACE2’s role in the renin-angiotensin system may add to the understanding of why there is increased morbidity and mortality among those with preexisting hypertension or other co-morbidities [7]. Understanding SARS-CoV-2’s mechanism helps us understand the pathophysiology of the disease process and therefore the most likely therapies. As far as antiviral medications to combat the ARDS picture, we are searching as quickly as possible. HIV medications are being tried; oseltamivir has not been found to be beneficial. Anti-malaria meds such as chloroquine may show promise [8]. We are innovating and improvising. The mounting pandemic scarcities and fears are all too real, but our agility and ability to change directions at a moment’s notice keeps us fighting as best we are able.
COVID-19 presents a significant health and economic threat to our global society. It will continue to evolve in unpredictable ways before the print publication of this article. Though we have seen many similar viruses make the jump from animal vectors to human-to-human transmission, the community transmission threat of this virus is incredibly high. We, as a healthcare community, must continue to stay informed and continue to practice protection of ourselves. An agile and adaptable approach is also our realistic and pragmatic approach, as COVID-19 is neither the first nor the last emerging viral disease that we will fight as a global health threat. ■
Editor’s Note: The number of current cases was last updated April 7, 2020.
References
- Coronavirus COVID-19 Global Cases by Johns Hopkins CSSE. Johns Hopkins University. Accessed April 7, 2020
- Field Briefing: Diamond Princess COVID-19 Cases. National Institute of Infectious Diseases, Japan. Published February 19, 2020. Accessed February 27, 2020
- Coronavirus Disease 2019 (COVID-19). Centers for Disease Control and Prevention. Updated February 29, 2020. Accessed March 2, 2020
- Florida Department of Health, Office of the State Surgeon General. Declaration of Public Health Emergency Executive Order Number 2020-51. Released 1 March 2020
- Salim Rezaie, “Surviving Sepsis Campaign Guidelines on the Management of Critically Ill Adults with COVID-19”, REBEL EM blog, March 22, 2020.
- N van Doremalen, et al. (2020). Aerosol and surface stability of HCoV-19 (SARS-CoV-2) compared to SARS-CoV-1. NEJM. doi: 10.1056/NEJMc2004973
- Hoffmann, M., et al. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell (2020). doi.org/10.1016/j.cell.2020.02.052
- Gautret P, et al. (2020). Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial. International Journal of Antimicrobial Agents. doi: 10.1016/j.ijantimicag.2020.105949
This article is part of the following sections:
Samantha manages fcep.org and publishes all content. Some articles may not be written by her. If you have questions about authorship or find an error, please email her directly.